Your body is a fascinating and complex organism that adapts to the stresses of any new environment to keep you alive. By exposing yourself to bursts of stress like Data-Driven Fasting, your body can adapt to thrive.
Your body is an adaptable marvel, and through Data-Driven Fasting (DDF), you’re about to witness its incredible capacity to thrive in a changing environment. DDF starts with simplicity, but as you journey further, curiosity might lead to questions.
This section delves into common inquiries that arise as you venture into the world of tracking and optimizing your blood sugar.
- 7.1 What Is A ‘Good’ Trigger Value?
- 7.2 What Is the Optimal Blood Sugar Level for Fat Burning?
- 7.3 What Is a Healthy Waking Glucose Level?
- 7.4 What Is Dawn Phenomenon?
- 7.5 How Does ‘That Time of The Month’ Affect Blood Glucose for Women?
- 7.6 Why Does My Blood Glucose Fall After I Eat?
- 7.7 Why Would My Blood Glucose Rise After a Low-Carb, High-Protein Meal?
- 7.8 Will Fasting Help My Gut Health?
- 7.9 How is DDF Different from Zoe or Day 2?
- 7.10 What Is the Glucose Ketone Index (Or Dr Boz Ratio)?
- 7.11 Will Data-Driven Fasting Help Me Lose Weight If I Don’t Have Diabetes?
- 7.12 How Can I Optimise My Sleep with Intermittent Fasting?
- 7.13 How Much Should My Blood Glucose Rise After a Meal?
- 7.14 Do I Need to Worry About ‘Insulin Toxicity’?
- 7.15 How Long Will It Take to Train My Hunger?
- 7.16 What If My Blood Glucose Rises Again Before I Eat?
- 7.18 Why Is My Waking Blood Sugar the Highest of The Day?
- 7.19 Why Do I Get Cold When Fast?
- 7.20 Why Do I Get Headaches When I Fast?
- 7.21 Why It’s More Important to Manage Your Basal Insulin Than Your Bolus Insulin
- 7.22 Why Your Goal is Not Flatline Blood Glucose Levels
- 7.23 What Happens to Glucose and Fat When We Eat?
- 7.24 How Can I Mitigate Menopausal Weight Gain?
- More
7.1 What Is A ‘Good’ Trigger Value?
We find it interesting to see how we compare with everyone else to understand how far we must go to catch up with others.
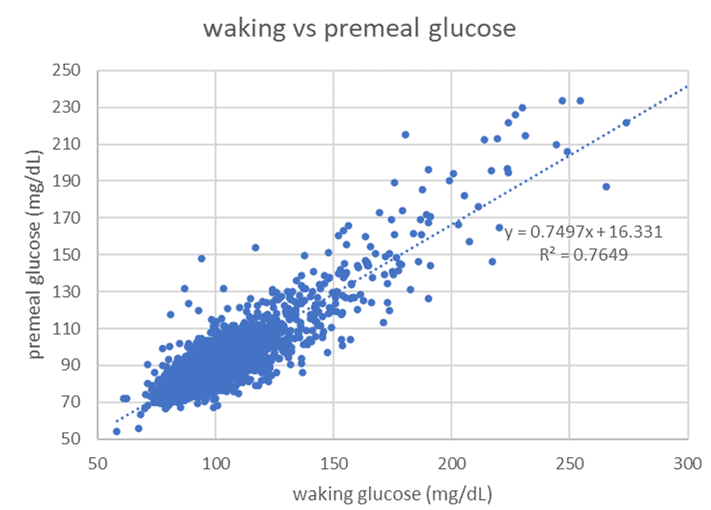
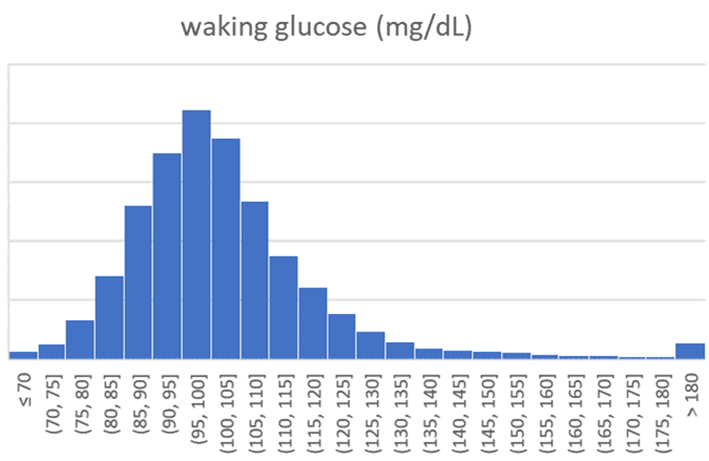
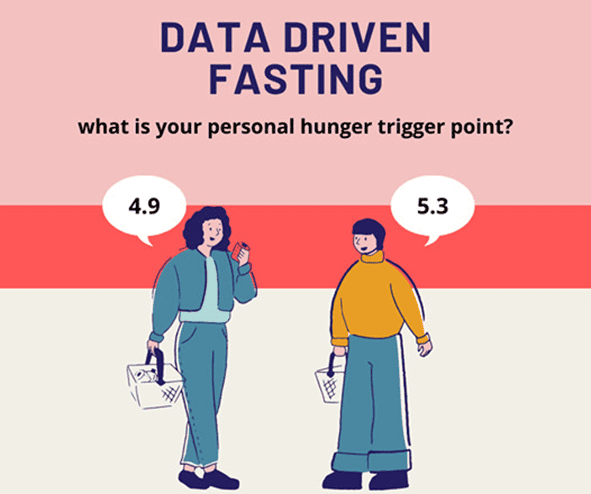
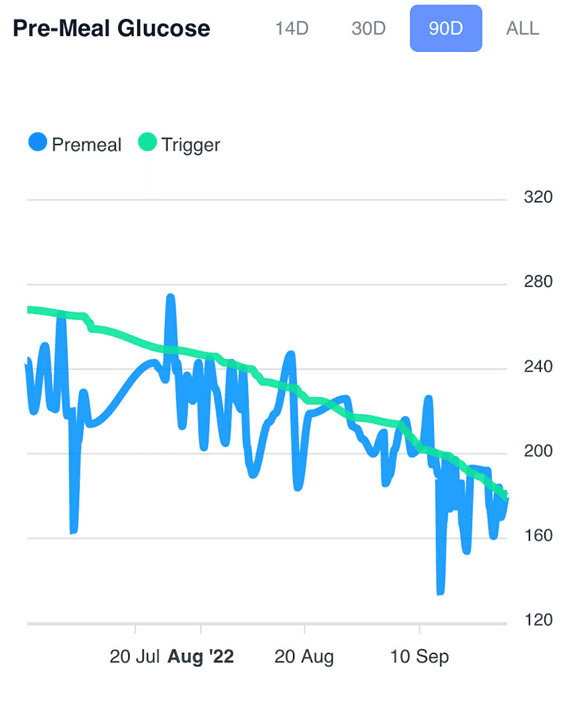
The chart below shows waking glucose vs. pre-meal trigger values logged in the DDF app (in mg/dL). As you manage your pre-meal trigger value, your waist, body fat, and waking glucose levels will follow.
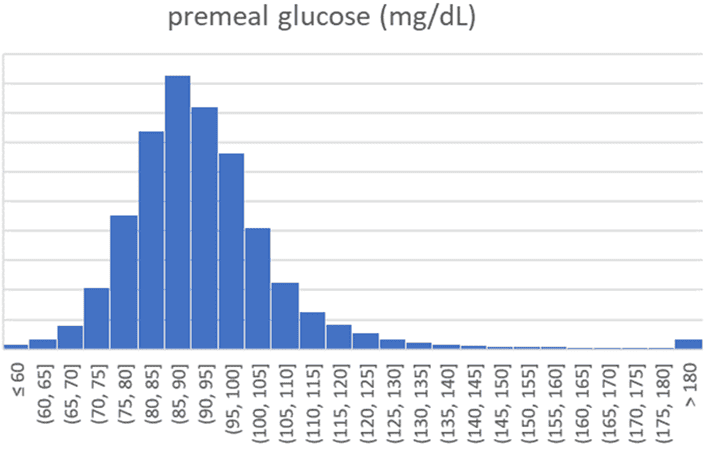
The chart below shows the distribution of pre-meal glucose values (in mg/dL) logged in Data-Driven Fasting Challenges.
The following chart illustrates the same data in mmol/L for those outside the US.
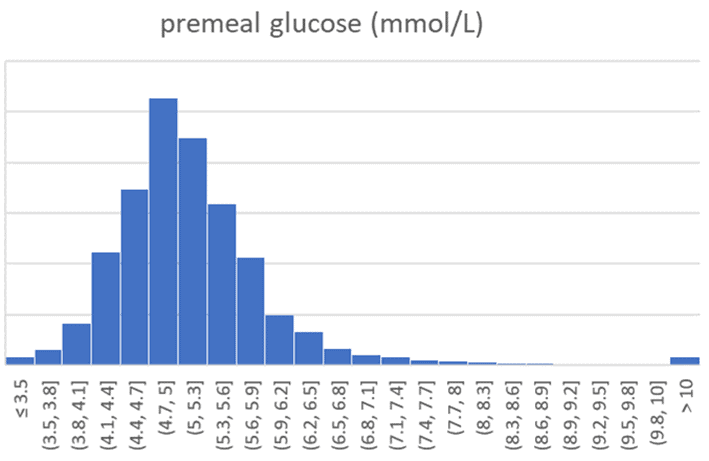
The table below summarises the analysis of 241,405 pre-meal blood glucose values.
| mg/dL | mmol/L | |
| Average | 82 | 4.6 |
| 15th | 76 | 4.2 |
| 85th | 88 | 4.9 |
| n | 251,405 | 251,405 |
- The average pre-meal glucose is 82 mg/dL (4.6 mmol/L).
- You’re likely metabolically healthy and fairly lean if your pre-meal blood glucose is towards the lower end of this range (i.e., close to 76 mg/dL or 4.2 mmol/L).
- However, if your pre-meal blood glucose is on the upper end of this range (i.e., closer to 88 mg/dL or 4.9 mmol/L or above), you may have some more work to optimise your metabolic health.
For more detail, see What are Normal, Healthy, Non-Diabetic Blood Sugar Levels?
7.2 What Is the Optimal Blood Sugar Level for Fat Burning?
You are constantly burning a combination of fat and glucose. We tend to burn more glucose when doing an intense activity and more fat during rest or lower-intensity activities.
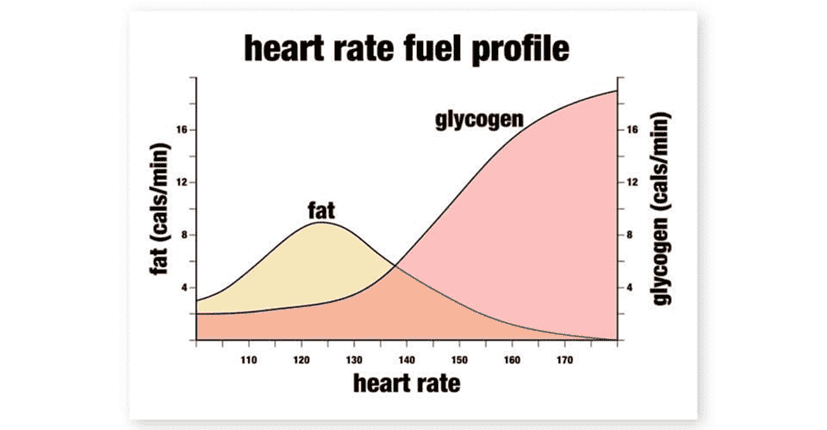
But if you have a lot of glucose in your system, you won’t burn as much fat because your body must burn through the glucose first because of oxidative priority.
As you lower the glucose in your system, your body will use more fat for fuel. So long as your dietary fat intake is not excessive, more of the fat you’re using for fuel will be from your body.
Counterintuitively, when we measure respiratory quotient, we find that people who are obese and insulin-resistant tend to primarily burn glucose at rest despite having a lot of fat on their bodies.
As you wait until your glucose drops below your Personalised Trigger before you eat, you will ensure that you burn more fat at the end of each fasting period. As you slowly lower your premeal trigger through repeated cycles of short-term ‘fasting’ and nutrient-dense feasting, you will burn more fat and less glucose as you drain excess glucose backed up in storage.
As the glucose in your blood and glycogen in your liver drop, your body will turn to your stored body fat for fuel. Therefore, as long as you are not supplying excess dietary fat, you will burn body fat when your glucose levels are lower.
7.3 What Is a Healthy Waking Glucose Level?
While most of us focus on weight and body fat, being below your Personal Fat Threshold is arguably more important. But how do you know if you are below your Personal Fat Threshold?
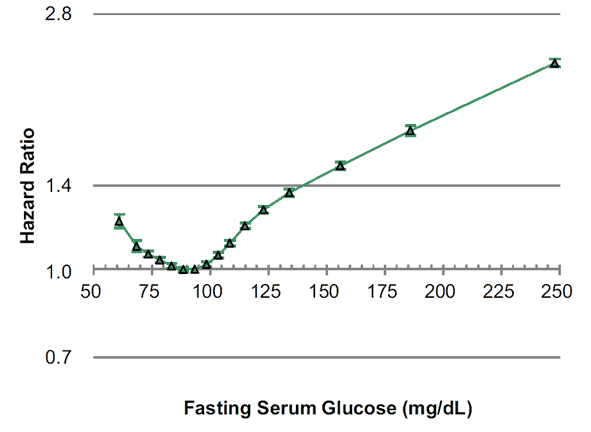
As you can see from the chart below (from Association between fasting glucose and all-cause mortality), the lowest overall risk of dying from any cause aligns with a fasting glucose between 80 and 100 mg/dL (4.4 to 5.6 mmol/L).
If your waking blood glucose is in this optimal range, it means:
- you are insulin-sensitive,
- your insulin levels are low,
- your body fat can absorb extra energy from your food and
- you do not have excess energy backing up into your bloodstream.
The charts below show the distribution of waking glucose numbers recorded in the DDF app (in mg/dL and mmol/L).
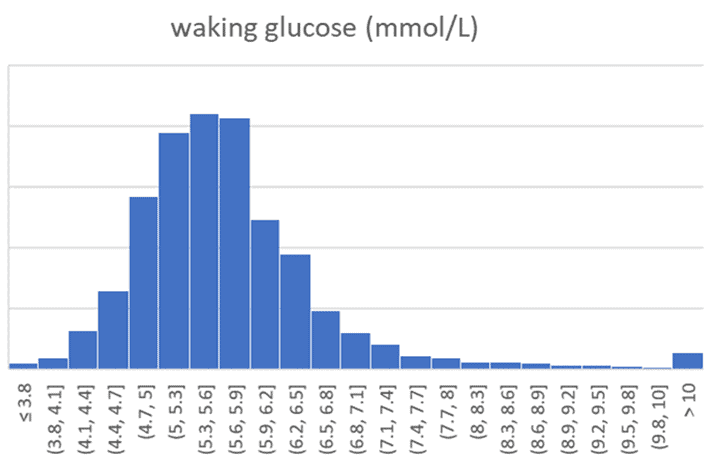
The table below shows the average waking glucose, along with the 15th and 85th percentile values.
| mg/dL | mmol/L | |
| average | 103 | 5.7 |
| 15th | 88 | 4.9 |
| 85th | 116 | 6.4 |
| n | 124858 | 124858 |
It’s important to note that lower waking glucose isn’t necessarily better. While rare, very low waking glucose (e.g., below 76 mg/dL or 4.2 mmol/L) corresponds to anorexia, poor immunity and fragility.
Additionally, your waking glucose may be slightly higher than ‘optimal’ if you follow a lower-carb diet. However, your glucose across the day will tend to be lower. Conversely, people on the lower fat diet tend to see lower waking glucose but higher glucose values across the day.
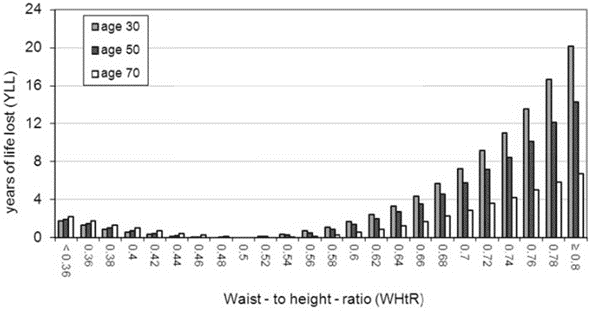
Keep in mind that waking glucose is just one of the parameters that you can use to gauge your overall metabolic health. Body fat % and waist-to-height ratio are also valuable markers to understand your overall level of metabolic health. Below 25% body fat for women and below 15% for men is a great goal, while a waist-to-height ratio of less than 0.5 is ideal. But, again, pushing significantly below these levels may not be healthy or sustainable.
You can track your waking glucose in the DDF app as a marker of metabolic health. However, it’s not critical to the DDF process and does not affect your trigger.
You may see your waking glucose increase as insulin drops, your stored energy is released, and you start to lose weight. Later, you may see your waking glucose stabilise at a lower level once you switch to Maintenance Mode.
Waking glucose isn’t something you can easily “hack”. Lower waking glucose follows as you chase a lower premeal glucose trigger, lose body fat and improve your overall metabolic health.
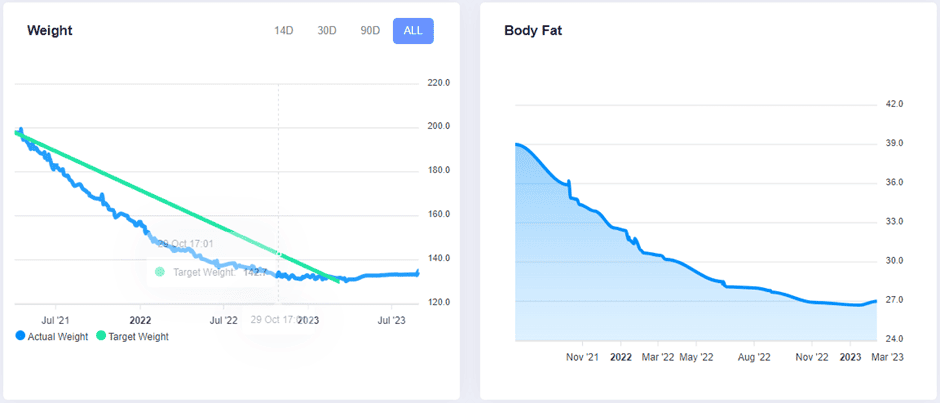
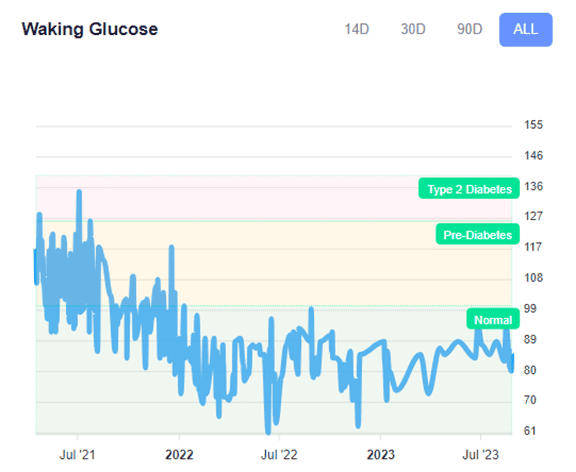
To illustrate, the chart below shows Muffy’s waking glucose over three years of using the DDF app. To achieve this, she simply chased a lower premeal glucose over successive rounds of DDF challenges.
As she chased a lower trigger, the weight dropped at around 1% per week for over a year, and her waking glucose followed the trend. For more, see From Struggles to Triumph: Unveiling Muffy’s Inspiring Journey to Optimal Health and Wellness.
7.4 What Is Dawn Phenomenon?
Your body clock (i.e., circadian rhythm) is closely tied to your eating, sleeping, activity, and light exposure.
As your body prepares to wake, melatonin decreases while cortisol and adrenaline rise. Your body releases glucagon from the liver to increase the glucose in your bloodstream, so you are fuelled and ready to bounce out of bed and start the day.
This increase in glucose is stimulated by glucagon and is usually balanced by insulin. This duo ensures your blood glucose is regulated and doesn’t rise too much. People with Type-1 Diabetes typically see their insulin requirements the lowest overnight, with a rise a few hours before they wake up as their liver pushes out glucose to start the day.
People with some degree of insulin resistance may find that their blood glucose increases more in the morning due to what is known as the Dawn Phenomenon. While some rise in glucose in the morning is normal, increased insulin resistance means that the glucose released from the liver is not balanced with insulin to stabilise blood glucose.
There is no need to eat immediately if your blood glucose is high in the morning, especially if you are not hungry. But when you start to feel hungry, rather than waiting until your blood glucose is below your trigger, you can choose to have a higher protein meal.
Prioritising protein earlier often causes blood glucose to fall, and you can eat again sooner rather than waiting all day. As you draw down on your excess fuel, you will see your waking blood glucose come down and a smaller rise due to the dawn phenomenon.
For more details, see Waking Up with High Blood Sugar? It Might Be the Dawn Phenomenon.
7.5 How Does ‘That Time of The Month’ Affect Blood Glucose for Women?
Females of reproductive age should be aware that cravings, blood glucose, and insulin sensitivity vary throughout the month.
Women with Type-1 Diabetes find their insulin requirements increase in the days leading up to their period before dropping once menses commences. In addition, insulin requirements rise after ovulation until a few days before menses commences.
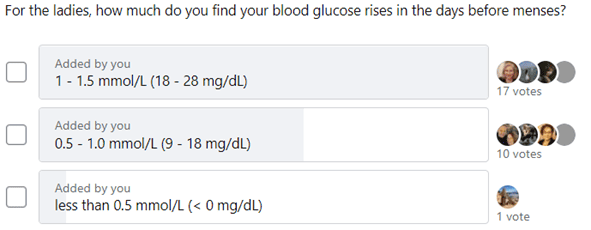
Insulin requirements and blood sugar rise between ovulation and menses as progesterone rises. The chart below shows the variation in total daily insulin requirements for my wife Monica over 34 monthly cycles.
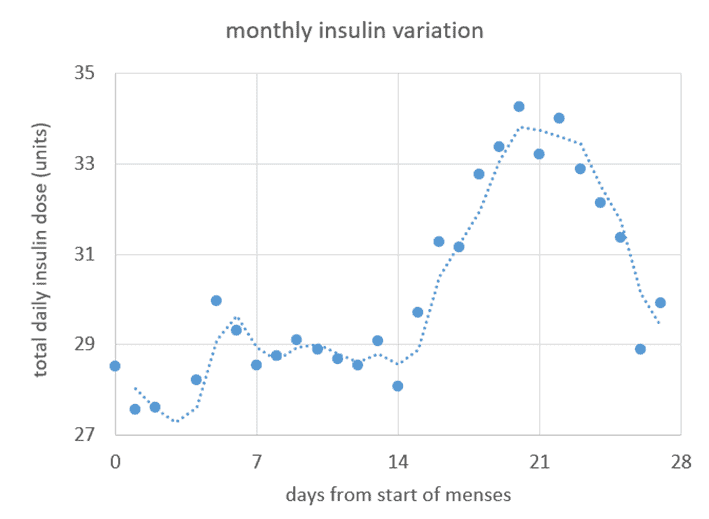
Cravings, water retention, and associated water weight gain also increase in the days leading up to menstruation. So, you may need to be more gracious with yourself when waiting for your blood glucose to drop if it’s ‘that time of the month’. Your body is preparing for a possible pregnancy and craving more energy and nutrients, particularly protein.
You may want to accept a slightly higher trigger value or default to your regular eating routine and eat when you are hungry during this time rather than fighting the process too much.
The DDF app will allow you to log ‘menses’ when you log a pre-meal trigger value. This will give you a temporarily elevated trigger, so you don’t have to battle with your trigger unnecessarily during this time.
For more discussion, see What to Eat for Each Phase of Your Monthly Menstrual Cycle.
7.6 Why Does My Blood Glucose Fall After I Eat?
Some people are surprised that their blood glucose drops after eating. This is a positive sign that you are metabolically healthy or not overeating carbohydrates.
Because glucose and fat stores in your liver are depleted after an overnight fast, many people see their blood glucose drop after their first meal. Any energy they eat goes to replenish the stores in their liver rather than backing up into their bloodstream.
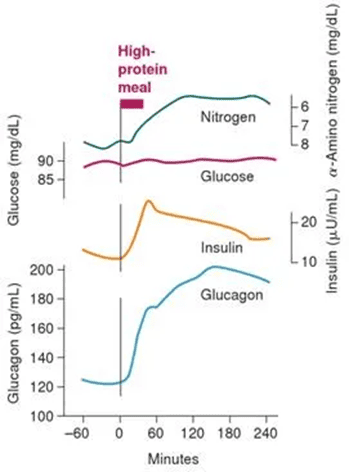
When you eat a higher protein meal, your pancreas secretes some insulin to enable you to use the amino acids to repair muscles and organs, make neurotransmitters, and a host of other functions. Glucagon is also released by your pancreas to balance insulin, as shown in this chart (from Marks’ Basic Medical Biochemistry).
For someone below their Personal Fat Threshold, this balance of insulin and glucagon means that blood glucose will generally remain stable. Blood glucose may even decrease, indicating that you have plenty of spare capacity to absorb the meal you just ate and that energy from your meal is not overflowing into your bloodstream.
Testing your glucose response to a high protein meal can be a useful measure of insulin resistance vs. insulin sensitivity and whether you are above your Personal Fat Threshold. You know you’re reasonably metabolically healthy if you see your blood glucose drop after a high-protein meal.
Conversely, if you see your blood glucose rise, you may have some level of insulin resistance. However, the solution is not to avoid protein. Instead, it would be best to reduce carbs and fat while prioritising protein to decrease your body fat levels below your Personal Fat Threshold.
For more details, see Why Does My Blood Sugar Drop (or Rise) After Eating Protein?
7.7 Why Would My Blood Glucose Rise After a Low-Carb, High-Protein Meal?
Someone who is insulin resistant or has diabetes has (i.e., insufficient insulin to maintain stable blood glucose). This person may see their blood glucose rise after a high protein meal as glucagon kicks in to tell the liver to release stored glycogen. Insulin is also released to keep blood glucose stable.
If someone is insulin resistant, their insulin does not work effectively, and their blood glucose is not suppressed. Therefore, insulin-resistant people can see a rise in blood glucose after a high-protein meal because they have insufficient insulin to simultaneously metabolise the protein and suppress glucagon release from their liver.
Some people see this rise in glucose and think they should avoid protein to maintain stable blood glucose. However, this may make things worse.
If you are insulin resistant (i.e. Type2 Diabetes) or your pancreas is not producing enough insulin (e.g., Type-1 Diabetes), your pancreas is not producing enough insulin to suppress gluconeogenesis, so you lose excess protein via gluconeogenesis (i.e. protein is converted to glucose). If this is the case for you, you will likely benefit by focusing on a higher protein percentage to ensure you don’t have to overeat to get the protein your body needs.
If you are insulin resistant because you carry excess body fat, the solution is to focus on foods with a higher protein percentage to increase satiety. This will enable you to lose body fat without losing too much lean mass.
If you are already lean (i.e., waist:height ratio less than 0.5) and you see elevated blood glucose after a low-carb, high-protein meal, talking to your doctor to measure your fasting insulin and c-peptide may be helpful. This will help you understand if your pancreas can produce enough insulin to rule out Type-1 Diabetes or MODY (Maturity Onset Diabetes of the Young).
For more details, see Keto Lie #4: Protein Should Be Avoided Due to Gluconeogenesis.
7.8 Will Fasting Help My Gut Health?
While adjusting to solid food after fasting for multiple days can be challenging, many people find intermittent fasting improves their digestion and gut health.
When we eat more food more often than we need to, our gut struggles to keep up, and we get indigestion and bacterial overgrowth. Conversely, when we eat less, we give our stomachs a chance to rest. The excess ‘bad bacteria’ (e.g., Firmicutes) associated with obesity die off as they are not continually overfed with nutrient-poor inflammatory foods. As a result, the ‘good bacteria’ (e.g., Bacteroidetes) associated with healthy body weight can flourish.
Gut health is complex, and there is still a lot to learn. You can’t analyse your faeces to determine what to eat. What we do know, however, is that:
- Eating ultra-processed foods that combine refined starches, sugars, and industrial seed oils will cause an overgrowth of ‘bad bacteria’ and excess growth in the human host.
- Prioritising nutrient-dense, high-satiety foods will help you eat less often, leading to a more balanced gut bacteria and a leaner human host.
7.9 How is DDF Different from Zoe or Day 2?
There seems to be a technological arms race to create a patented system to provide personalised nutrition recommendations based on the analysis of your poop.
Zoe is a technology start-up company spearheaded by Professor Tim Spector that seeks to provide personalised nutritional advice based on gut microbiome analysis.
To get your personalised nutritional prescription from Zoe, you send your ‘poo in the post’ to their lab for analysis (USD$350, plus USD$59 for app access after six months). You also test your glucose (using a CGM) and fat response to standardised low-fat and high-fat muffins.
While the well-funded Zoe team are publishing fascinating data, this level of testing and analysis is potentially excessive for most people.
Day 2 is a similar service that provides meal recommendations based on your stool analysis. Their work is based on a 2015 study Personalized Nutrition by Prediction of Glycemic Responses, which identified that people could have markedly different glucose responses to the same food. Therefore, they hypothesised that they could design a diet to stabilise blood sugars based on a complex (and patented) analysis of your gut bacteria.
There is no doubt some interaction between your blood sugars, body weight, and microbiome. However, the relationship between the three is incredibly complex. It’s impossible to tease out correlation vs. causation and determine how to use this data to guide dietary choices. The experts haven’t yet defined a ‘good vs. bad’ microbiome profile, let alone what to eat to improve yours.
No matter how much data or computing power is applied to the task, we may never reach the point where anyone can tell you what to eat by looking at what goes down the toilet. Without an intelligent application of a fundamental understanding of how your body uses energy from your food, particularly how your glucose and fat fuel tanks interact, we risk paralysis by analysis and falling victim to garbage in – garbage out (GIGO).
As shown in the figure below from the Zoe PREDICT 1 study, despite the hype, your gut microbiome is NOT a strong predictor of your glucose or fat response to food. Instead, meal composition, genetics, meal context, and current blood sugar levels have a more significant effect than your microbiome.
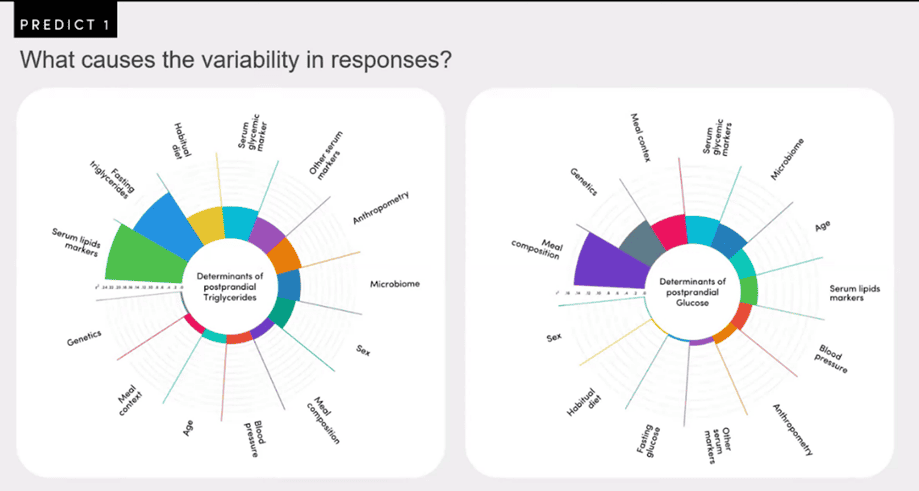
What we can see from the PREDICT1 study data is that:
- the macronutrient composition (i.e., the mixture of carbs, fat, and protein) of food has the most significant impact on your blood glucose response to a meal, while
- the amount of fat already in your blood has the most significant impact on the rise in the fat in your blood after you eat. If your system is already full of energy, there is nowhere for the extra energy to go.
This aligns with our understanding of how glucose and fat fuel tanks work in our bodies. If your fat stores are full, excess fuel cannot be absorbed, backs up in the system, and overflows in your bloodstream.
If you eat in a way that gives your body the nutrients from the food that it needs to function and attain a more optimal body composition, your gut bacteria will likely ‘improve’ as it continually adapts to the food you feed it.
While there will always be some variability in your glucose response to the foods you eat, our analysis of the Food Insulin Index data gives us a solid understanding of factors affecting our short-term insulin and glucose responses to foods. We have used this understanding to identify optimal foods and meals suited to a wide range of goals and preferences that will allow you to stabilise your glucose to healthy levels.
Rather than prescribing a meal plan and recipes designed for someone else, the DDF app allows you to track your glucose response to the foods you eat to empower you to create a shortlist of meals you enjoy eating that work for your unique metabolism.
In the Data-Driven Fasting 30-Day Challenge, we use simpler, less invasive, and more cost-effective biometrics to guide your dietary choices.
- If your blood sugars after meals rise by more than 1.6 mmol/L (30 mg/dL), reduce your intake of processed carbs until your blood sugars stabilise.
- If your waist-to-height ratio is > 0.5 and your blood sugars are in the healthy range after dialling back carbs, you will likely need to cut back on your fat intake.
Not only will your blood sugars and body composition improve as you stop overeating, but your gut microbiome will become healthier, too.
7.10 What Is the Glucose Ketone Index (Or Dr Boz Ratio)?
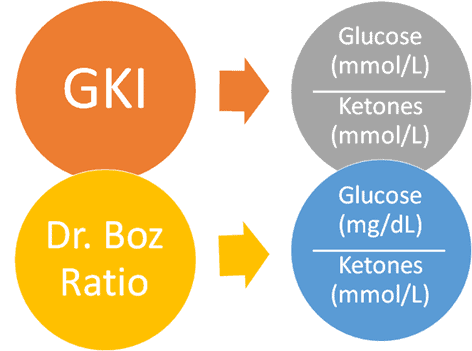
The Glucose:Ketone Index (GKI) was developed in 2015 by cancer researcher Professor Thomas Seyfried to track cancer patients’ metabolic health while fasting for prolonged periods.
The GKI is your glucose (in mmol/L) divided by your ketones (in mmol/L). More recently, Dr Annette Bosworth has popularised the Dr Boz Ratio, glucose (in mg/dL) divided by ketones (in mmol/L).
Use of the GKI is based on the understanding that if glucose is low and ketones are high, insulin levels will be low, and you’re in good metabolic health. Conversely, your insulin levels are likely high if your glucose is high and ketones are low when you fast. This indicates that you have some level of insulin resistance that you need to attend to.
The problem, however, comes when people don’t differentiate between:
- endogenous ketones that are made from your body fat when you’re fasting vs
- exogenous ketones that are from the fat in the food you just ate, added MCT oil, or ketone supplements.
Most of the benefits that are often attributed to ketosis come from the energy deficit. If you are jamming in thousands of empty calories of nutrient-poor fats to raise ketones to get a higher GKI or Dr Boz ratio, then you will be driving up insulin levels as your pancreas has to work overtime to hold the added energy in storage.
You will likely be producing plenty of ketones from your body fat if you are chasing a lower pre-meal blood glucose. You don’t need to worry about measuring ketones because they don’t give you any guidance about what or when you should eat. We recommend you skip the expense and confusion of testing ketones and focus on pre-meal blood sugars.
For more detail, see Is the Acetone:Glucose Ratio the Holy Grail of Tracking Optimal Ketosis?
7.11 Will Data-Driven Fasting Help Me Lose Weight If I Don’t Have Diabetes?
Data-Driven Fasting will work for most people trying to lose weight, even if they don’t meet the criteria for diabetes.
While Type-2 Diabetes is diagnosed when you have a fasting glucose of greater than 125 mg/dL or 7.0 mmol/L, you can use Data-Driven Fasting to drive your pre-meal trigger down to much lower levels (e.g., 70 mg/dL or 3.9 mmol/L). As you do this, your weight and body fat levels will follow.
While using your glucose to guide what and when you eat is extremely helpful for people with Type 2 diabetes, most of the people in our challenges have glucose values in what would be considered the normal healthy range. Rather than settling for ‘normal’ the DDF Challenge guide people to optimise their metabolic health and weight.
The one scenario where Data-Driven Fasting may not be as effective is when people have been on a high-fat, low-protein ketogenic diet for a long time. These people may already have very low blood sugars, which don’t vary much after eating, but still have a lot of fat to lose. In this scenario, our Macros Masterclass tends to be more effective in helping them fine-tune their macros to suit their goals (e.g., prioritise protein and reduce fat to facilitate fat loss).
7.12 How Can I Optimise My Sleep with Intermittent Fasting?
Not eating too late in the day seems to help us sleep better. According to Professor Matthew Walker in his book Why We Sleep, we don’t enter REM sleep while burning off a lot of energy from a late dinner.
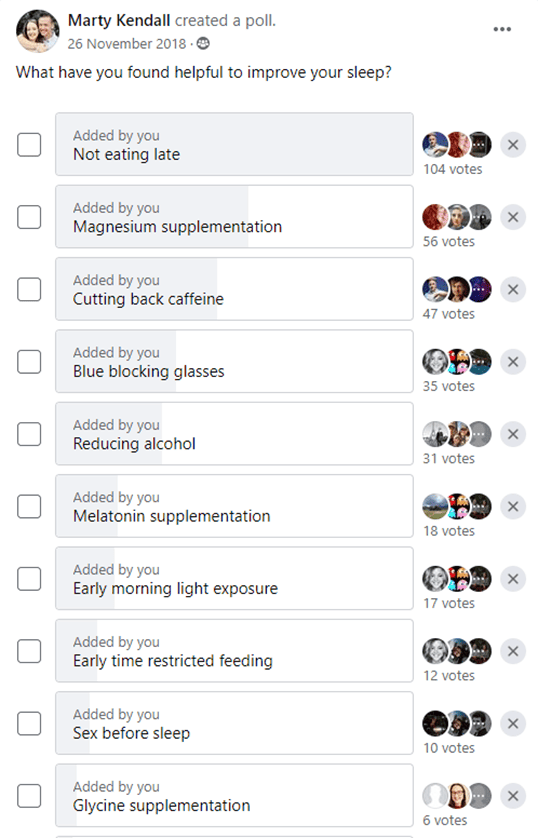
This survey of Oura Ring users shows that not eating too late is the most beneficial ‘hack’ to ensure sound sleep based on their quantitative data.
Don’t be surprised if you find you sleep more soundly as your blood glucose decreases because your body is not working so hard to process excess energy overnight.
On the flip side, it’s also good not to be too hungry when you go to bed. If you find you wake up through the night because you are hungry, you may need to eat something a bit closer to bedtime or make your dinner a little larger. A little carbohydrate at your last meal may be beneficial to raise glucose into the normal range to ensure your body doesn’t think it’s starving overnight.
Your body prioritises burning off alcohol, which can keep your metabolic rate elevated. So, try to avoid too much alcohol later at night. Similarly, protein requires a lot of energy to metabolise, so it’s ideal if you don’t try to consume all your daily protein too close to bed. In contrast, carbs and fat are metabolised more easily (i.e., they have a lower Dietary Induced Thermogenesis) and thus will give you a better chance at a sound sleep.
7.13 How Much Should My Blood Glucose Rise After a Meal?
Data-Driven Fasting primarily focuses on blood glucose before meals to ensure you are reducing the excess energy stored in your body. As insulin sensitivity improves, waking and post-meal blood glucose should also decrease.
If you see your blood glucose rise by more than 30 mg/dL or 1.6 mmol/L in the one to two hours after you eat, you likely ate too much or too many carbohydrates at that meal. You should either avoid that meal or eat less of it in the future. Your glucose tank is already full, so you don’t need more carbs.
Many people find their blood glucose rises more after dinner, indicating that their energy stores are being overfilled. As a result, they may benefit by reducing the size of their dinner and prioritising larger meals earlier in the day when their energy tanks are not as full.
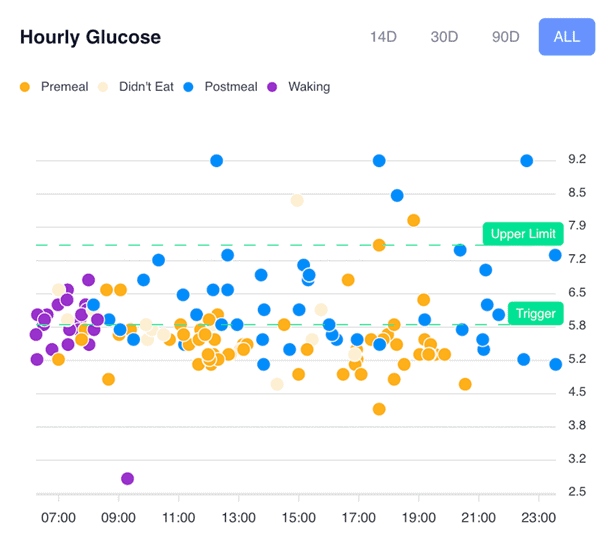
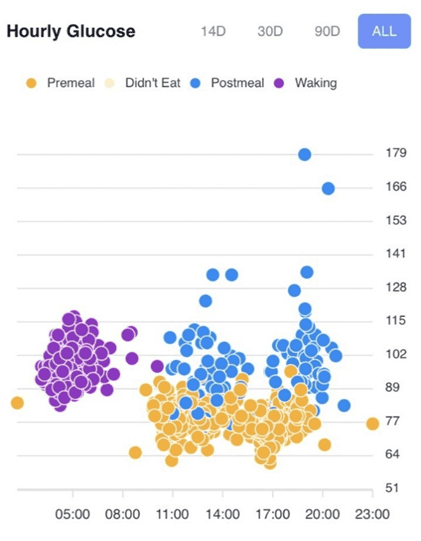
You can use the hourly glucose charts in the DDF app to tailor your meal choices and routine to minimise the post-meal glucose values above the upper limit line (i.e., 1.6 mg/dL or 30 mg/dL). Once you master this, you can focus on your pre-meal blood sugars and delay your meals to reduce your trigger.
The rise in glucose after you eat is more a reflection of what you ate. On the contrary, your fasting blood glucose and your glucose before meals indicate your metabolic health and whether you are over-fuelling throughout the day.
7.14 Do I Need to Worry About ‘Insulin Toxicity’?
Many people focus on insulin toxicity as the ‘root cause’ of diabetes and metabolic disease. Hence, they see reducing insulin as the end goal.
However, if you are part of the 98.5% of the population with a functioning pancreas that is not injecting insulin to manage Type 1 Diabetes, your body won’t produce more insulin than required to keep body fat in storage when food is coming in from your mouth.
When someone with Type-1 Diabetes accidentally injects too much insulin, their liver will aggressively slow the release of energy into the bloodstream, and their blood glucose will drop quickly. This causes them to feel ravenously hungry, and they will be driven to eat anything and everything to bring their blood sugar levels back up.
However, unless you are either a Type-1 or insulin-dependent Type-2 diabetic injecting insulin, high insulin levels do not cause overeating or obesity. The reverse is true: overeating causes obesity and high insulin levels. Therefore, rather than worrying about ‘insulin toxicity’, we should focus on managing energy toxicity, and insulin will look after itself.
The Carbohydrate – Insulin Hypothesis simplistically assumes:
carbs -> insulin -> fat storage
However, it is a little more complex than this. It’s critical to understand the true cause-and-effect relationship. Rather than addressing the symptoms of high insulin, we need to focus our effort and attention on the root cause. A rise in insulin is simply the response to increased body fat. It is not the cause! Instead, the real cause is:
low satiety, nutrient-poor foods -> increased cravings and appetite to get the nutrients we need -> increased energy intake -> fat storage -> increased insulin
Hence, the solution to managing diabetes, blood glucose, and insulin levels and dodging the complications of metabolic syndrome is:
high–satiety, nutrient-dense foods and meals -> decreased cravings and appetite -> decreased energy intake -> fat loss -> lower insulin levels
You will reduce your body fat by managing your pre-meal blood glucose by waiting to eat until you need to refuel. As a consequence, your insulin levels will also fall.
We designed Data-Driven Fasting to keep things as simple as possible by shifting your primary focus to blood glucose before meals to draw down on glucose and fat stored in the body, reducing your insulin levels throughout the day.
For more details, see:
- What Does Insulin Do in Your Body?
- How to Reverse Your Insulin Resistance,
- Your Metabolism Explained: In 2 Infographics, and
- What Is Insulin Resistance (and How to Reverse It)?
7.15 How Long Will It Take to Train My Hunger?
People with elevated blood glucose often find it hard to judge their true hunger. So, monitoring blood glucose is a great way to train your hunger if you are overweight or have elevated blood glucose.
Many fascinating studies (e.g. Training to estimate blood glucose and to form associations with initial hunger) have shown that people can learn to predict their blood glucose from their sensations of hunger.
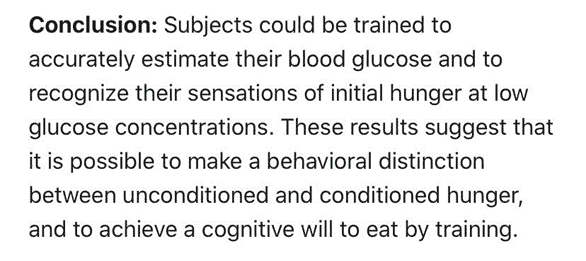
After several weeks of testing blood glucose, people can get a good feel for their blood glucose when they are truly hungry based on their symptoms, like their stomach rumbling, changes in energy levels, becoming food-focused or mental fatigue.
When you log your blood glucose in the DDF app, it’s critical to take a moment to observe your hunger and log your current hunger level. This moment of self-reflection is critical to help you calibrate your hunger signals.
Once you can predict your blood glucose and rate your hunger based on your symptoms, you will be able to wait until you are hungry to eat. From there, you can wean yourself off the measuring and rely on your hunger signals.
For more detail, see Hunger Training… How to Use Your Glucometer as a Fuel Gauge to Train Your Appetite For Sustainable Weight Loss.
7.16 What If My Blood Glucose Rises Again Before I Eat?
The goal of Data-Driven Fasting is to use your blood glucose to validate your hunger before you eat.
If your blood glucose is below your trigger when you feel hungry, you have successfully depleted the glycogen in your liver and have begun to use more body fat. You are ready to refuel again!
However, when they test again before they eat, some people have found that their blood glucose may have risen while preparing their meals. It is normal for your body to release glucose into your bloodstream:
- when it anticipates food is coming,
- as part of the normal process of maintaining stable blood glucose and
- if it gets stressed by low blood glucose and hunger.
The ‘secret’ here is not to test again. Go ahead and eat if you are hungry and your blood glucose has dipped below your trigger, and you were hungry.
This is one of the downsides we see with people using continuous glucose monitors, as it can provide more data than necessary. In Data-Driven Fasting, we want to use the minimum effective dose of measurement to ensure you move progressively rather than become overwhelmed and give up before you reach your goal.
7.18 Why Is My Waking Blood Sugar the Highest of The Day?
If you have plenty of stored body fat, your body will release it as energy overnight into your bloodstream, even if you follow a lower-carb diet.
Your body can make glucose from protein and even the fat you eat and the fat on your body. So, if you have excess energy stored in your body, the glucose you’re consuming from food will back up in your system and overflow into your bloodstream.
Making sure you are not overeating too late may help decrease waking blood sugars. However, reducing your body fat levels to more optimal levels may take some time. To do this, you need to keep chasing a lower pre-meal blood sugar by delaying your meals. You also must ensure you are eating nutrient-dense, high-satiety meals when you do eat.
Counterintuitively, people on a higher-fat diet often see higher blood glucose levels in the morning, particularly when they ate more fat the night before.
If your waking glucose is elevated, you could experiment with eating less fat in your evening meal. Over time, by using your blood glucose to guide what and when to eat, you should find that your blood glucose levels become more consistent across the day.
For more details, see Waking Up with High Blood Sugar? It Might Be the Dawn Phenomenon.
7.19 Why Do I Get Cold When Fast?
Some people find that one of their symptoms of lower blood sugar is being cold. This is because when your body has less fuel available, it slows the amount of energy it uses to save energy.
You should take this as a sign that you are hungry and ready to eat. If there is food available, your body won’t let you be cold and miserable for too long before your appetite kicks in and you wake Lizzy.
If you feel cold regularly, you should ensure you are getting adequate protein when you eat. Not only does protein help you maintain your precious muscle, but it also produces more heat as you digest and metabolise it (i.e., the thermic effect of food).
7.20 Why Do I Get Headaches When I Fast?
As well as energy, your body stores toxins in your body fat. As you lose weight, these stored toxins will flow into your bloodstream and need to be processed and excreted by your kidneys. People who fast for extended periods can get bad headaches to these toxins, which overload the body and often drive them to eat sooner.
If you are getting headaches, you should make sure you are drinking plenty of fluids. Some electrolytes (e.g., salty water or our Optimised Electrolyte Mix recipe) can also help when your body excretes electrolytes when your blood sugars drop.
With Data-Driven Fasting, headaches are rare unless they are losing more than 1.0% per week. Losing between 0.5 and 1.0% per week is sustainable and allows your body to process and clear the toxins.
7.21 Why It’s More Important to Manage Your Basal Insulin Than Your Bolus Insulin
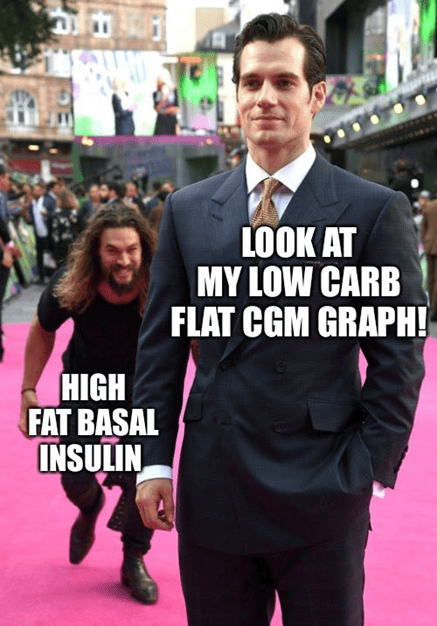
Unfortunately, confusion and misunderstanding abound regarding the role of insulin in our bodies. Unfortunately, optimising our blood glucose, insulin, and body fat is not as simple as reducing our intake of carbohydrates to achieve more stable blood sugar levels.
Insulin is an important and powerful hormone secreted by the pancreas. Its most well-known role is to facilitate the movement of glucose from the bloodstream into your cells, to either be used as energy or stored away.
The graph below from the Food Insulin Index Data shows how different foods raise our insulin levels after eating (postprandial).
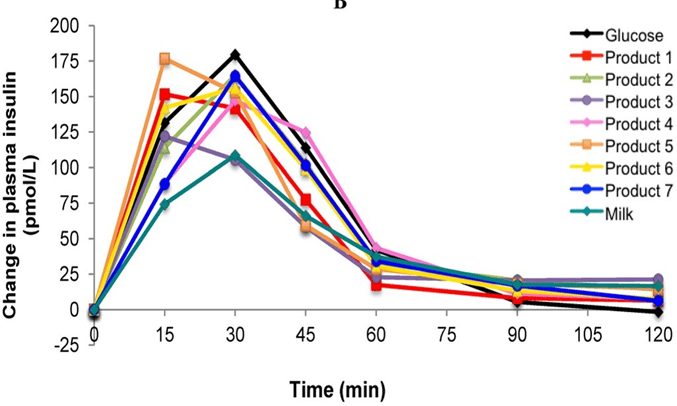
Notice that pure glucose (black line) quickly drives insulin up, then returns to baseline after two hours. In contrast, foods like milk (containing a combination of fat and carbs) have a small initial spike but keep insulin levels elevated beyond the two-hour mark.
But the more significant but often overlooked role of insulin is to function as a dam, holding back your stored energy while dietary energy is coming in through your mouth. Another useful analogy is to view insulin as the bake pedal to signal to your liver to slow the release of stored energy.
Monitoring insulin dosing of people with Type 1 Diabetes using insulin pumps gives us a fascinating insight into the actual magnitude of ‘basal insulin’, which is required to stop your body from disintegrating — regardless of whether you are eating. In contrast, bolus insulin refers to increased insulin levels after eating.
In people on a standard Western diet, basal insulin makes up about half their daily insulin dose. However, basal insulin can be 80-90% of the daily insulin requirement for people adhering to a low-carb or keto diet.
A recent study of people with Type 1 Diabetes showed that when insulin wasn’t taken:
- dietary glucose raised blood sugar in the first three hours or so, while
- dietary fat initially lowered blood glucose in the short term but caused a significant rise after three hours.
So, rather than focusing on carbs vs fat or fasting for days at a time, you need to find a way to reduce the amount of energy from your food sustainably. This allows your body to reduce the amount of energy you’re holding in storage and thus reduce your insulin levels throughout the day.
7.22 Why Your Goal is Not Flatline Blood Glucose Levels
Because the amount your blood glucose rises after meals is closely related to what you eat, many people think managing their blood glucose levels after meals is their end goal. They mistakenly believe that super-stable, flat-line blood sugars will improve their metabolic health and promote fat loss.
Unfortunately, this misguided thinking leads some to swap carbs for more dietary fat and even less protein. This often results in a nutrient-poor, low-satiety diet that drives the pancreas to increase basal insulin levels and, thus, total insulin across the day.
Simply swapping carbs for fat in an effort to pursue flat-line blood sugars and lower insulin is a bit like measuring the volume of water in the ocean by measuring the height of the waves at the beach. To extend this analogy, swapping carbs for fat is akin to stopping the wind to make the waves smaller. Meanwhile, focussing on our premeal glucose moves us from high tide to low tide to lower the overall energy in our system.
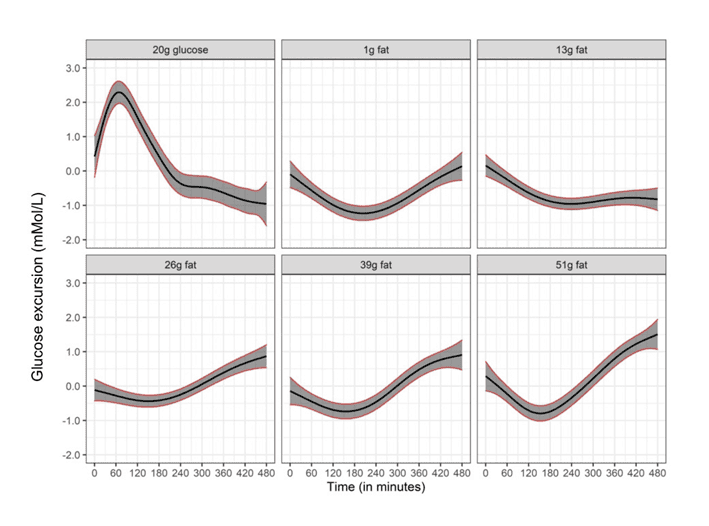
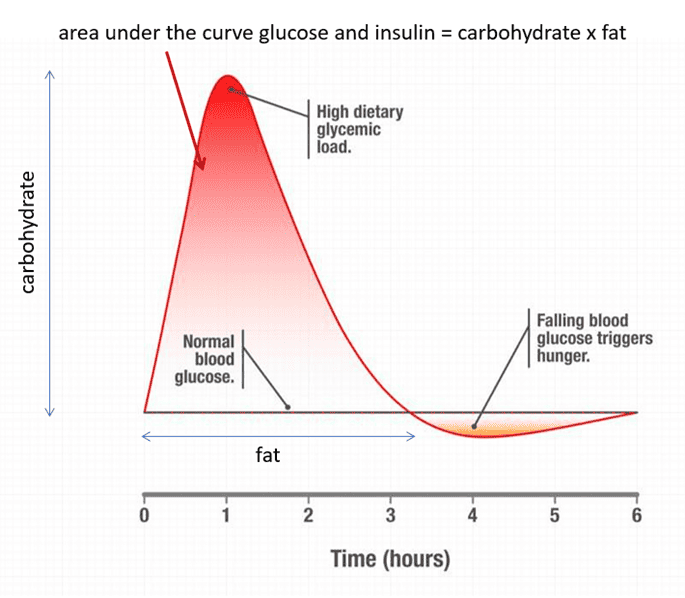
The real solution is to reduce the area under the curve of your insulin and glucose levels throughout the day, not just after you eat! As shown in the image below, dietary carbohydrate governs the short-term rise in glucose, but dietary fat prevents your blood sugar from dropping for longer.
The only way to get your blood sugars to drop below what is typical for you and access your stored energy is to progressively dial back the energy from fat and carbs in your diet and wait to eat until your body needs more fuel.
Data-Driven Fasting uses the insights from your blood sugars to guide you through fine-tuning:
- when,
- what, and
- how much you eat.
Before long, you learn to select higher-satiety foods that empower you to manage your appetite, enabling you to eat less and use stored energy for fuel.
Our analysis of 487,285 glucose values from 4,402 people who have used our Data-Driven Fasting app over the past two years shows that your blood glucose before you eat matters the most. Once you solve the energy toxicity problem (i.e., excess stored energy), insulin toxicity and all the other downstream issues related to your metabolic health will look after themselves.
For more details, see What are Normal, Healthy, Non-Diabetic Blood Sugar Levels?
7.23 What Happens to Glucose and Fat When We Eat?
In a recent study (Hall et al., 2020), NIH researchers fed participants a 75% fat or a 75% carbohydrate diet for two weeks. They tracked blood glucose continually and tested free fatty acids present in the participants’ blood after meals.
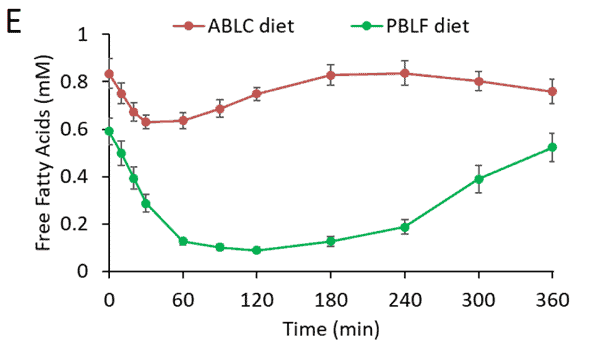
The chart below shows how free fatty acids change after a low-fat meal (plant-based low fat – green line) vs. a high-fat meal (animal-based low carb – red line). Fat in the blood decreases more after a high-carb meal as the liver (controlled by insulin) slows the process of ‘lipolysis’ (the release of stored fat) until all incoming dietary energy is exhausted. Once our bodies clear the carbs, stored fat is again released into the bloodstream.
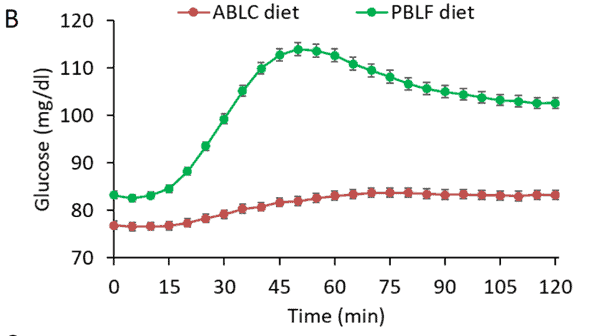
The following chart from the same study shows that after eating a high-carb meal (plant-based low-fat – green line), blood glucose levels rose for about an hour and then fell back towards the baseline, while a low-carb, high-fat meal (animal-based low-carb – red line) elicited a much flatter glucose response. Interestingly, participants lost slightly more weight on the low-fat diet despite their higher glucose and insulin levels.
Unfortunately, dietary advice promoted by some keto advocates (i.e., reducing carbs and protein and increasing dietary fat) only manages one symptom by stabilising blood glucose after meals; it won’t necessarily help you lose body fat or reverse insulin resistance.
As shown in the chart below from our analysis of people using Data-Driven Fasting, there is no correlation between a smaller blood glucose rise and a healthier waist-to-height ratio.
So, while overfilling your glucose fuel tank with more dietary carbohydrates than your body requires is not a great idea, swapping carbs for fat to achieve more stable blood sugars doesn’t help address the root cause.
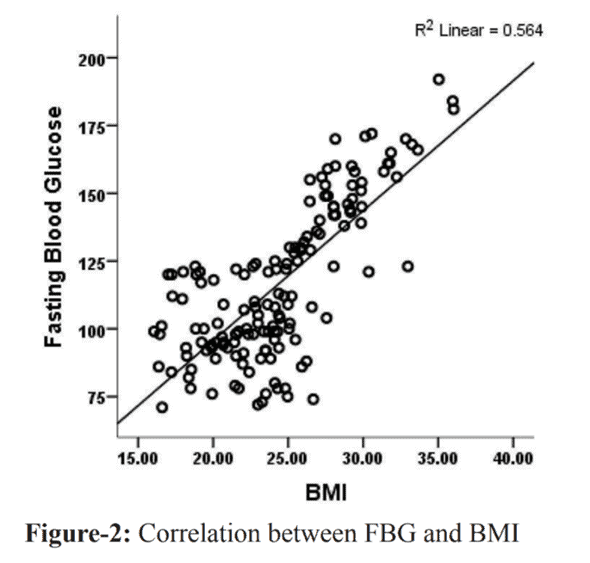
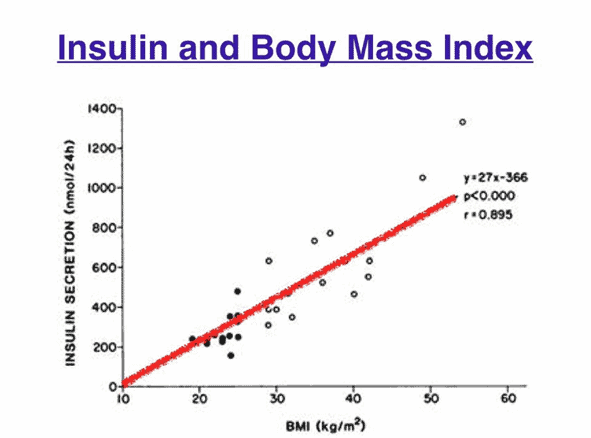
The charts below show that body fat (assessed by the Body Mass Index or BMI), insulin, and blood glucose have a strong positive correlation. Therefore, the higher your body fat, the higher your fasting blood glucose and insulin across the day are likely to be.
So, the only meaningful way to reduce your insulin and fasting blood glucose levels and reverse Type-2 Diabetes is to reduce the amount of stored body fat you are carrying.
To learn more, see:
- How to use a continuous glucose monitor for weight loss (and why your CGM could be making you fat), and
- How to lose weight using a continuous glucose monitor (CGM) and Data-Driven Fasting.
When you don’t eat for a while, your body begins to use up the fuel available in your bloodstream (i.e. both the glucose and fat).
As these supplies are depleted, your liver releases glucose to maintain stable blood sugars. Then, as glycogen stores are exhausted, your body uses a process known as ‘gluconeogenesis’ to convert protein and even fat to glucose to refill your liver. This critical process ensures that you always have some glucose available for explosive activity if required!
When your glycogen stores are depleted—but not entirely exhausted—your blood glucose starts dropping. Then, finally, you begin pulling energy from stored body fat.
Congratulations. It now takes less insulin to ‘hold’ your fat in storage.
Whether you’re eating a high-fat or a high-carb diet, the key to burning stored body fat is having blood glucose levels return below your baseline before eating again.
7.24 How Can I Mitigate Menopausal Weight Gain?
Many women find they gain weight during menopause and turn to fasting and other aggressive strategies to improve their body composition. However, sadly, extended fasting and extreme calorie restriction may be exacerbating the problem.
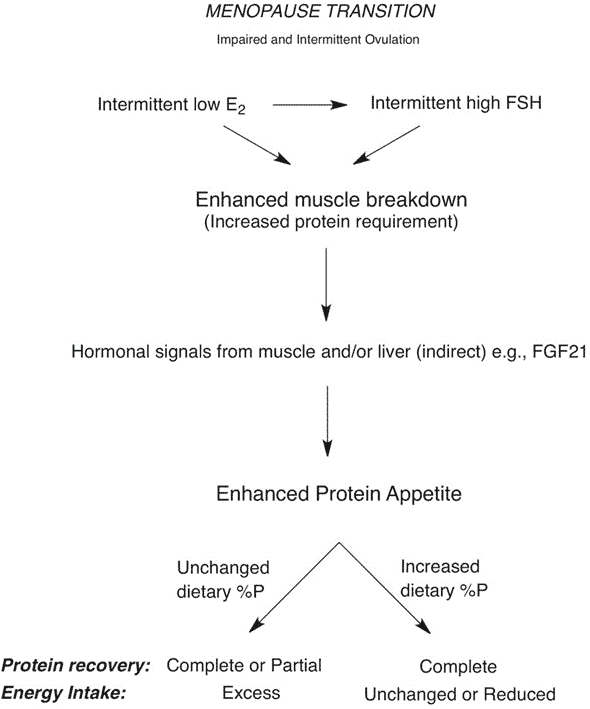
A recent study, Weight gain during the menopause transition – evidence for a mechanism dependent on protein leverage, by Professors Raubenheimer and Simpson outlined the mechanism and the solution.
During menopause, women experience a reduction in estrogen and increased anabolic resistance/insulin resistance (which also occurs in men), leading to a loss of lean mass as we age. In addition, activity levels often also decrease as we age, so we require less food.
The body craves more protein to compensate for the loss of critical muscle mass. So, if we don’t change what we eat, we consume more food to get the required protein and hence gain weight.
To mitigate menopausal weight gain, we need to increase the protein % of our diet by dialling back energy from fat and carbs and prioritising protein. Of course, being more active is also helpful. But if you’re unable to exercise, you may need to increase your protein % a little more.
Most people think it’s the young bros that need more protein. However, they often find it easier to get adequate protein because they are more active and use more energy. We often see older women with the highest protein % thriving in our programs.
Data-Driven Fasting will guide you to prioritise protein and reduce energy from fat and carbohydrates when your blood glucose indicates you have plenty of energy available in your system. This will ensure you minimise the loss of lean muscle mass while also losing unwanted body fat and draining excess glucose.
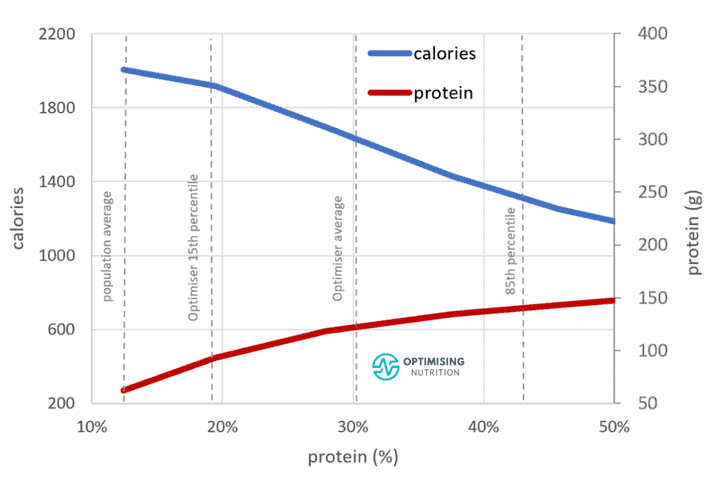
In their paper, Raubenheimer and Simpson emphasised that it doesn’t take a massive shift in protein % to mitigate menopausal weight gain. As shown in the chart below from our satiety analysis, increasing protein % tends to align with a considerable reduction in calories but only a moderate increase in protein intake.
One of the issues identified by the authors in the consultation with industry groups was that menopausal women wouldn’t know how to modify their diet to moderately increase their protein %. While this sounds simple, in theory, it’s often challenging to change our habits and fight against our instincts to crave energy-dense foods that provide energy from fat and carbs and less protein. Many people come unstuck when they try to jump from one extreme to another.
Often, tracking your food for a few weeks can be helpful. If you need some extra help, this is the exact process we guide Optimiser through in our four-week Macros Masterclass.
For more, see Menopausal Weight Gain: The Problem and Solution Explained and our Menopausal Weight Loss QuickStart Guide.
More
- Data-Driven Fasting: How to Use Your Blood Glucose as a Fuel Gauge
- Join the next Data-Driven Fasting Challenge
- Try the Data-Driven Fasting app
- Get the DDF Manual
- Join Our Community
- DDF QuickStart Guide
- The DDF app User Guide
- Frequently Asked Questions
- Results
- Articles


Marty–look what I found this morning…this kinda sorta validates what you say about data driven fasting: https://www.sciencedaily.com/releases/2021/04/210412114802.htm
the Zoe study demonstrates that people eat more when they get super hungry when their BG dips too much before they eat. DDF solves that problem for a fraction of the price and without the hassle of wearing a CGM or sending your poo in the post. see https://optimisingnutrition.com/understanding-your-unique-metabolism-ddf-faq-part-7/#htoc-7-9-how-is-ddf-different-from-zoe-or-day-2
“If your liver is already stuffed full of glycogen, it can take a few weeks to deplete. ” Doesn’t your liver only contain a few hundred kcal of glycogen, something like a few hours supply of energy for your body? Why would it take a few weeks to deplete?
because it is constantly refilled from your diet and even GNG from the glycerol backbone of your fat stores. it takes a few weeks to drop in a sustainable manner that doesn’t lead to rebound binging because your glucose plummets to below what you are used to.