Are you caught in the web of blood sugar management, insulin fears, and weight loss confusion? You’re not alone. In the ever-evolving world of health and nutrition, myths and misunderstandings persist. We’re here to unravel the truth.
If you’ve ever believed that the path to weight loss and metabolic health involved flattening your blood sugar with a high-fat diet, hold on tight. The journey we’re about to embark on will challenge these notions and reveal the key to optimizing your metabolic health.
Join us on a data-driven exploration, from understanding insulin’s role in your body to deciphering the difference between Type 1 Diabetes and the rest of us. Discover the surprising reality of insulin resistance, explore the science behind insulin, and learn why stable blood sugars might not be the ultimate goal.
We’ll dig into glucose variability, the importance of pre-meal blood sugar, and how the “what” you eat matters as much as “when” you eat. By the end, you’ll have a clearer picture of how to unlock your metabolic health and achieve your weight loss goals.
So, let’s dive in and separate fact from fiction on this fascinating journey through the intricacies of blood sugar, insulin, and weight loss.
BONUS: Download Free Data-Driven Fasting Book That Has Helped Thousands Of People Personalize Their Fasting Routine
- Our journey
- What we know from people with Type 1 diabetes
- How insulin really works
- The difference between people with Type 1 Diabetes and everyone else!
- But what if I’m “insulin resistant”?
- Is insulin REALLY the problem?
- Show me the science!
- The most important markers to manage
- Flatline CGM envy… Why are we still chasing the wrong numbers?
- How much should my blood sugars rise after a meal?
- Stable glucose does not equal fat loss!
- Glucose variability
- Premeal Trigger
- Doesn’t WHAT I eat matter too?
- The bottom line
Our journey
Eighteen years ago, I married Monica, who has Type 1 Diabetes.
We started to think about having kids. But she knew she needed to get her blood sugars under control to minimise the long list of dire complications of pregnancy with high blood sugars.
She has lived with Type 1 Diabetes since she was ten years of age. But sadly, no endocrinologist or diabetes educator had ever been able to tell her what to eat or how to manage her insulin dosing to help her gain control of her diabetes.
The conversation always went along the lines of…
Endo: “Your blood sugars and HbA1c are high. You should try to get that down.”
Monica: “How doc? What do I do? What do I eat? What do I change?”
Endo: “It just needs to be better. Here’s your script for insulin and drugs. See you in six months.”
Luckily, when we were looking at having kids, we found a progressive doctor who taught us enough enable Monica to get reasonable control for our two pregnancies. Back then, we learned about matching carbohydrates to insulin dosing and how to fine-tune insulin sensitivity. Seventeen years later, they seem to have turned out OK.

Later we found the Type One Grit Facebook Group, which follows Dr Richard Bernstein, and our life changed radically (for the better).
Bernstein was an engineer who later became a doctor after he got frustrated at people not listening to his theories about diabetes management that he discovered after analysing his own blood sugars. He’s now 85 and going strong. He continues to walk the talk.
Recently, we had to see an endocrinologist and a diabetes educator get a new insulin pump for Monica so we could set up a closed-loop CGM/insulin delivery system. The conversation with both of them went along the lines of:
“Wow. What a fantastic HbA1c! I don’t think I can teach you anything! You know what you’re doing… But wait. Your chart says you haven’t seen an endocrinologist for seven years. What?!?!”
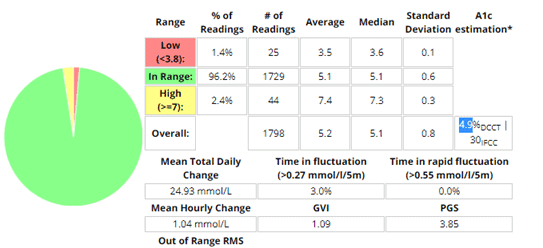
Over the past few months we have been able to use the closed loop CGM system, combined with wise dietary choices, to achieve even better blood sugar control.
And a non-diabetic HbA1c of 4.9%!
I have learned a lot after diving deep into the Type 1 Diabetes headspace. I also learned that context is critical, especially if you are part of the 99.985% of the population who has a functioning pancreas.
Before I get into the data analysis and learnings from people using Data-Driven Fasting, let me give some background to help you understand the difference between people with Type 1 Diabetes and the rest of us.
What we know from people with Type 1 diabetes
Injecting large doses of insulin to treat elevated blood sugars from modern processed food leaves them on a blood sugar rollercoaster. When their blood sugars are high, they inject more insulin to bring them down.
A few hours later, when they find they have overshot their blood sugar target. They are ravenously hungry and will eat anything and everything until they can raise their blood sugars again. A day in the life of most people living with Type 1 Diabetes looks like this.

Injected insulin is driving their appetite.
If their insulin doses are not precisely matched with the food they eat (which is nearly impossible with synthetic injected insulin combined with synthetic, processed food), they end up overeating because of the insulin they are injecting.
Living with rollercoaster blood sugars sux. Your appetite, mood or energy levels are in the toilet!
To be clear, whether you are injecting insulin or not, you don’t want to have wildly oscillating blood sugars. When they come crashing down below your normal baseline levels, you will feel super hungry and compelled to overeat.
People who are metabolically healthy tend to see their blood sugars rise by less than 1.6 mmol/L or 30 mg/dL after meals. So you ideally want to cut back on carbs (to avoid overfilling your glucose fuel tank) to achieve blood sugars in the normal healthy range.
However, swinging to the other extreme and simply replacing all carbohydrates with refined fat (and even avoiding protein) to achieve flatline blood sugars does not address the root cause of type 2 diabetes/metabolic syndrome/insulin toxicity. It’s largely just symptom management, not the cure.
How insulin really works
While we usually think of insulin as the hormone that forces energy into our cells, it’s not the full story.
Proponents of the Carbohydrate Insulin Hypothesis like to think of insulin as a “miracle-gro for your fat cells“.
While this is a compelling metaphor, suggesting that we will grow fatter just by eating carbs, irrespective of energy balance, it is incorrect and fundamentally misguided.
We all have approximately 5 grams of glucose (or 20 calories worth) buzzing around in our body at any one time (i.e. about a teaspoon’s worth). It doesn’t take long to use this up once we turn off the flow of energy into our bloodstream.
If you could turn off the release of energy from your liver completely, you would run out of glucose completely in about 15 minutes.
Insulin is the hormone, secreted by the pancreas, that reduces the flow of energy into your bloodstream (from your liver and adipose tissue) until you burn up the energy in your blood from that last meal.
But rather than thinking of insulin as an anabolic hormone that helps things grow, it’s much more useful to think of insulin as anti-catabolic (i.e. stops us from breaking down and disintegrating).
As per Dr Bernstein’s Law of Small Numbers, once people with Type 1 Diabetes reduce the inputs that require larger doses of insulin (i.e. processed carbohydrates), they can stabilise their blood sugars and insulin requirements.
Smaller inputs of carbs and insulin with meals lead to smaller errors that are easier to correct throughout the day. Then, because they are no longer injecting excessive amounts of insulin to treat the blood sugar roller coaster, their appetite stabilises, and they tend to achieve healthy body fat levels.

Rather than rollercoaster blood sugars with poor appetite control (which drives an energy surplus), they can have stable blood sugars and healthy appetite signals. If you are part of the 1 in 8000 people with T1D whose pancreas doesn’t work, stabilising your blood sugars and insulin should be your #1 priority!
The difference between people with Type 1 Diabetes and everyone else!
But, if you are part of the 98.5% of the population that is fortunate enough to have a functioning pancreas, EVERYTHING IS DIFFERENT.
You cannot turn off your insulin pump or stop taking insulin.
No matter what we believe, it just doesn’t work like that!
Your pancreas will always produce just enough insulin (no more, no less) to hold your body fat in storage until you have used up the extra energy from the food that is coming in from your mouth.
When you stop eating, insulin levels lower and your stored energy is allowed to be released for use.
If you have Type 2 Diabetes and eat a heavily processed diet of carbs and fat (e.g. modern processed junk food) your blood sugars will shoot up after you eat and take a long time to reduce back to baseline.
But what if I’m “insulin resistant”?
Many people have developed a victim mentality (I was one of them).
They blame their obesity on their insulin resistance.
They think being insulin resistant makes it harder for them to lose weight.
But, the reverse is actually true.
When you are lean and insulin sensitive, your body is only too willing to store energy and grow. A starving caveman or a lean bodybuilder after a show is highly insulin sensitive, ready to store every morsel they can get their hands on.
However, conversely, once you become insulin resistant, your body is only too willing to offload the excess energy as soon as you stop jamming in excess energy from low satiety nutrient-poor processed foods that are driving you to overeat them.
The chart below shows the difference between diabetic and healthy blood sugar levels (i.e. higher and with larger swings).
Foods that are a combination of fat+carb together enable your body to fill both fuel tanks at the same time. Because your fat stores are already full, the extra energy is not easily absorbed by your liver and body fat, so it overflows into your bloodstream.
You can’t blame getting fat on insulin. You’d die without it. You don’t really want to turn off your pancreas. Trust me – being an uncontrolled Type 1 Diabetic in ketoacidosis is not fun.
It’s the foods with carbs and the fat (with low protein) that caused you to overeat. Now you have lots of body fat that requires lots of insulin to hold in storage so long as you keep eating that food.
As you will see below, it’s not that stable blood sugars or a low carb diet is a bad thing. However, eating a high-fat diet to achieve stable blood sugars is largely symptom management.
Switching carbs for refined fat and avoiding protein won’t make you lean and metabolically healthy. It often makes things worse!
Is insulin REALLY the problem?
Over the past few years, people in the fasting/low carb/keto community have been told by doctors and nutrition gurus that insulin toxicity is the root cause of the majority of our western diseases.
Insulin is public enemy number one and reversing “insulin toxicity” is key to weight loss.
We don’t have a lot of data about our insulin response to the food we eat. But important to note that the data we do have (i.e. the Food Insulin Index data) only measures the response to foods over the first two hours (as shown in the chart below).
The limited duration of this data leads many people to think that high-fat foods have a negligible impact on insulin and hence they are effectively a “free food”.
While glucose will raise your insulin levels quickly, foods that contain fat and carbs together (like milk, shown by the aqua line) will have a smaller initial impact, but insulin will stay elevated well beyond two hours.
While we don’t know that much about the long term insulin effect of high-fat foods, it appears that they will keep our insulin levels elevated for longer. Because fat is stored more efficiently, you don’t need as much insulin to hold it in storage, on your bum and belly.
Your body wants to excess glucose quickly, so it raises insulin to abruptly halt the release of stored energy until you have burned it off. However, because your body can store massive amounts of fat there is no need to raise insulin as much. Your body is more than happy to store all the fat it can get for a possible famine.
Once we understand that insulin simply holds our stored energy back while we use up the energy coming in from our diet, we realise that ALL food will increase insulin over the long term. The problem is not insulin toxicity, but rather energy toxicity (that leads to increased insulin levels).
The bottom line: If we want to lose fat from our body, then it’s not merely a matter of eating fewer carbs and more fat.
Show me the science!
Since launching the Data-Driven Fasting Group, I have been bombarded with questions about blood sugars and insulin as people test their blood sugars and try to make sense of the data they see.
Why do my blood sugars rise when I don’t eat?
My blood sugars are flatline? Why am I still fat?
I thought it would be interesting to see what we could learn from this massive dataset.
The most important markers to manage
When it comes to metabolic health and longevity, there are three things we can easily measure that we collect in Data Driven Fasting:
- body mass index (BMI),
- waist to height ratio, and
- waking glucose.
As shown in the charts below of body mass index, waist:height ratio and waking glucose, lower is not always better. However, due to the constant availability of hyperpalatable nutrient-poor processed foods, most of us are well on the higher side of optimal.
Flatline CGM envy… Why are we still chasing the wrong numbers?
These days, I’m seeing more and more people (who don’t have Type 1 Diabetes) walking around with (expensive and often painful) continuous glucose monitors eating more fat and less protein and fewer carbs to maintain flat line blood sugars.
They post their flat-line blood sugars on Facebook and Instagram.
A few years ago it was ketone envy. Now it’s flatline CGM envy.
CGM technology is a Godsend for people (like my wife) who have Type 1 Diabetes and need to keep an eye on their blood sugars constantly. But, while everyone wants the latest gadget, for most people, more data is not better.
If you already have a CGM (or are considering purchasing one), you may be interested in checking out How to lose weight using a continuous glucose monitor (CGM).
How much should my blood sugars rise after a meal?
The table below shows the generally accepted limits for blood glucose after meals.

The key things to note here are:
- If your blood sugars after meals are elevated above 140 mg/dL or 7.8 mmol/L then you have prediabetes or diabetes and definitely need to work to reduce your post-meal blood glucose by reducing refined carbohydrates and/or medications to reduce blood sugars (e.g. insulin or metformin).
- A rise in glucose from 100 mg/dL to 140 mg/dL would be accepted as normal and healthy. If your blood sugars rise by less than 40 mg/dL or 2.6 mmol/L after meals, then you have a fully functioning pancreas, and you would benefit by focusing on your blood sugars before you eat if you have more weight to lose.
In the Nutritional Optimisation Masterclass and Data-Driven Fasting, we set even tighter limits than this. We recommend that people reduce the processed carbs in their diet if their blood sugars rise by more than 1.6 mmol/L or 30 mg/dL.
The chart below shows the hourly glucose chart from our Data-Driven Fasting app. In the first week of our Data-Driven Fasting Challenges, we guide people to dial back their carbohydrate intake to avoid overfilling their glucose fuel tank. But once you’ve ticked that box, you only need to focus on your premeal blood sugars to make progress.
The average blood sugar rise of people following Data-Driven Fasting is only about 10 mg/dL or 0.5 mg/dL (not much at all)! It seems people who are fans of fasting (and typically following a low-carb or keto diet) already have extremely stable blood sugars!
Stable glucose does not equal fat loss!
As shown in the charts below, people who have a higher waist:height ratio and BMI only have a slightly larger increase in blood sugar after they eat.

The correlation is extremely low (i.e. there is no relationship).

The correlation between the amount your glucose rises after you eat and your waking glucose (another key marker of metabolic health) is also non-existent.

It seems, while normal, healthy, stable blood sugars are a good thing, flat line is not better!
Although stable and lower blood glucose levels are a positive marker of metabolic health, merely treating the symptom (i.e. elevated blood sugar) rather than addressing the cause (i.e. insulin resistance, energy toxicity and excess body fat) doesn’t help.
Unfortunately, many people who believe that fat is a free food because it does not raise insulin levels end up overeating refined fat to maintain stable blood sugar levels. Before long, this leads to fat gain and worsening insulin resistance.
Sadly, there are plenty of keto gurus and their die-hard believers who continue to gain weight because they are trying to optimise the wrong numbers!
Glucose variability
When we look at glucose variability (i.e. standard deviation/average glucose), we see that there is also a negligible correlation between stable blood sugars and a better waist:height ratio, BMI or waking blood sugars.
Many people have combined fasting with a high-fat keto diet in an attempt to achieve stable blood sugars in the hope of weight loss. But sadly, in spite of their Herculean feats of self-deprivation, they continue to gain weight due to a low-satiety, nutrient-poor diet that leaves them craving and eating more when the fast is over. As shown in our survey in our Data-Driven Fasting Group, losing and regaining the same weight over and over is very common with popular fasting protocols.
Actively avoiding insulin and any normal rise in blood sugar levels using a high-fat diet tends to lead to poorer satiety, greater energy intake and obesity. In time, these people often end up with higher insulin levels across the day because they are carrying more body fat which requires more insulin to hold in storage.
Premeal Trigger
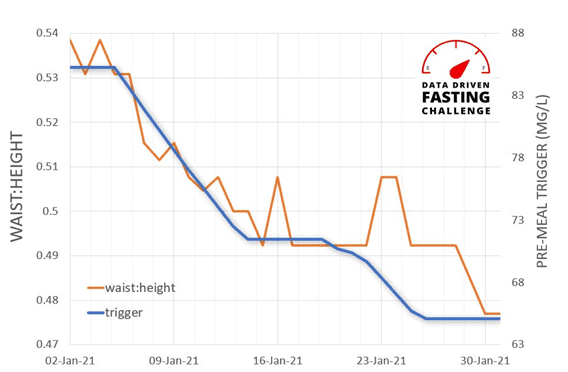
The good news is, we see a better correlation between pre-meal glucose and waist to height and BMI. Rather than worrying so much about your blood sugars after you eat, it seems that people who have a lower blood glucose before they eat tend to have much better metabolic health.

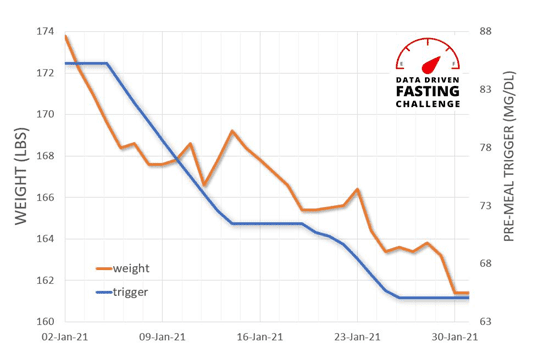
There is some variability across individuals due to different Personal Fat Thresholds. However, when we look at this person by person (e.g. Jane’s data below), we see that a lower premeal glucose trigger before you eat aligns nicely with weight, waist to height and body fat levels.
You can check out my interview with Jane (pictured below) here.
Your waking glucose is one of the most reliable indicators of metabolic health and your risk of dying from any cause.
As shown in the chart below, pre-meal blood glucose trigger strongly correlates with your waking glucose. Rather than worrying about the rise in glucose after you eat, managing your glucose before you eat is much more useful if you actually want to lose fat and gain health!

To optimise body composition, you need to measure and manage the things that matter. Your blood sugar before meals is a much more useful metric that you can manage by optimising your meal timing and intermittent fasting routine.
Doesn’t WHAT I eat matter too?
Yes. WHAT you eat is arguably more important than WHEN you eat.
Data-Driven Fasting simply empowers you to optimise your food timing to ensure a negative energy balance.
- While high-fat foods and meals will keep your blood sugars stable, they also provide a lot of energy and lower satiety. Although your blood sugars and insulin levels may be stable, your body won’t need to draw down on your body fat for a long time until it burns up all the energy from that fat bomb or buttered coffee.
- Meals with more fast-digesting non-fibre carbohydrates will raise your blood sugars quickly, but they may return to below baseline more quickly.
- Foods that contain both fat and carbs together (and low protein) will fill your fat and glucose fuel tanks at the same time and allow you to eat more and keep your blood sugars elevated for longer.
- Foods with a higher percentage of protein and a greater nutrient density are harder to overeat and won’t raise your blood sugars significantly (in fact, they may reduce them).
The bottom line
- Lower and stable blood sugar and insulin levels are a sign of good metabolic health, but managing the symptoms with a high-fat diet does not lead to metabolic health.
- The fundamental problem is not insulin toxicity. It’s energy toxicity.
- When you eat, rather than focusing on avoiding short-term blood sugar and insulin spikes, you should focus on high-satiety, nutrient-dense food that will reduce your cravings and allow you to lose body fat.
We designed Data-Driven Fasting to solve the energy balance problem and avoid the many pitfalls and shortcomings of calorie tracking. Using your blood sugars as a fuel gauge to return to just below your personal trigger ensures a long-term negative energy balance. Over time, insulin, blood sugars, waist, body fat and improved metabolic health will follow.
If you want to find Your Personal Trigger you can download our free baselining sheet here or download our free 130-page Data-Driven Fasting Manual here to learn all about how you can use Data-Driven Fasting to fine-tune your intermittent fasting routine to optimise your pre-meal blood sugars.
Learn more
- Download the (Free) Data-Driven Fasting Manual,
- Join the Data-Driven Fasting Facebook Group, or
- Join the next Data-Driven Fasting 30-Day Challenge.
- How to reverse type 2 diabetes and optimise your blood sugar
- Turning the Tide on Type 2 Diabetes: Real Stories of Reversal
- Keto Lie #10: Stable blood sugars will lead to fat loss
- What Does Insulin Do In Your Body?
Data-Driven Fasting Index
- Data-Driven Fasting
- Download the manual (PDF)
- Facebook Group
- QuickStart Guide
- Success stories & results
- FAQ #1 – What makes DDF different?
- FAQ #2 – Getting ready
- FAQ #3 – Tracking your progress
- FAQ #4 – WHEN to eat
- FAQ #5 – WHAT to eat
- FAQ #6 – Winning the mind game
- FAQ #7 – Understanding your unique metabolism
- FAQ #8 – Troubleshooting
- FAQ #9 – Things that affect your blood sugars (other than food)
- FAQ #10 – Moving on…
- Join the next 30-Day Challenge






I have been a type 2 diabetic for 20 years and I am trying to reverse it. I have lost 32kg an follow a low carb high fat / protein diet. I do not eat any refined foods. I have also stopped using insulin, but struggle to get my sugar levels down – even with fasting – 23 hour, 36 hour, 72 hour and longer.
We tend to find smaller bursts of ‘fasting’ guided by premeal blood sugars provide better long term results. Multi day fasting fasting tends to make it harder to prioritise food quality (i.e. adequate protein and micronutrients) when you eat. See https://optimisingnutrition.com/data-driven-fasting/ for some more details.
Brilliant. Looks to be very helpful, i will let you know.
thanks.
What absoulte bollocks.
Can you elaborate?
This made me chuckle. Are you sure Tim knows what that word means Marty? 😬
I’m eager to get some intelligent discourse on the topic. I think it’s sorely overdue! bring it on!
Fascinating. I think you may be on to something. I plan to experiment.
awesome! more details in this article. https://optimisingnutrition.com/data-driven-fasting/
Many foods are mineral deficient, and also many people’s digestive systems operate poorly, and these factors can cause the body to call for more food.
Definitely agree. A lack of minerals is a major driver of appetite. Have you seen our analysis here? https://optimisingnutrition.com/the-effect-of-minerals-on-hunger-and-satiety/
Whenever I read your analysis (+ this time also specifically as you commented on your wife’s journey through doctors) I wonder 1. why are we sending people to Mars, but can’t agree on how basics work in our body, 2. why do I need to read facebook to get valid help in living healthy life and can’t really talk to my doctor… Ranting aside – I definitely experienced with the help of NO Masterclass that the keto with the promise of “stuff yourself to satiety with fat” may not be working for me. That nutrition drives satiety. I still see something should be there with average insulin levels… I went from insulin 11 to 4 within the last few years and I do feel a big difference in how I’m feeling. I’m not that much different weight/fat level wise. It’s a pity we can’t measure insulin much more throughout days to really see. I was at morning BG of 84 with insulin 11, now I’m at 87 with insulin 4. So to me the fact that we can’t really measure insulin like we can BG is a bit of a blind spot, yet still with this blind spot the ideas you shared are definitely something that leads to a feedback loop that helps with healthy habits. You don’t water the flowers when they have wet soil. You don’t have to eat when blood glucose is high. I buy it.
thanks Dorota. we need to shift to focus on diets that allow us to reduce total insulin requirement across the entire day (not just after meals). T1D who can measure this on their pump is the only real way to do this.
Since diagnosis of T1D/LADA 17 years ago (age 47) I’ve always tested before eating. I typically use 5 units long-acting/day and 3-5 units/meal, with A1C in mid 6. My issue is I’m very slowly losing weight. A pound a year seems insignificant but adds up over 20 years (on an already small frame.) I can’t find anyone who addresses the issue of how to maintain weight; everyone else seems concerned about not gaining.
Rapid weight loss occurs in T1D without insulin. To reverse this you would need adequate protein and then dial up fat ‘as a lever’ to get more low satiety energy in. Check out this video from Dr B. https://www.youtube.com/watch?v=j4HkBDR_mcw
Sorry but no!
You absolutely totally forgot the oxidation of LDL particles by glycation when sugar level spiked or were present.
It is the fundamentals of all i formation and the primary reason for Coronary artery disease.
So keep your sugarow and balanced at all times.
Est more proteins because glucogenesis is not a problem and we all knowvit by now.
Keep Carbs as far as you can.
GL of 90 to 145 are perfectly healty and great
Make sure your A1c never passes 5.8 and you are healthy metabolically wise.
Oxidization of LDL occurs when we eat a modern processed fat+carb diet which leaves us with elevated fat and glucose in the blood. The point is stable blood sugars are good, but flatline is not necessarily better (at least if it requires a nutrient poor high fat diet). If you target the root cause (excess fat above your Personal Fat Threshold) you will address both high glucose and high fat in the blood.
I guess I’m just stupid. I’ve been a diabetic for over 2 decades. What idiot thinks measuring blood sugar after eating is a good idea? Blood sugar should be tested after fasting. I thought this was standard. As for most of this article…. um what? You are about as clear as mud. Cut to the chase. What are you saying?
1. Human metabolism is complex. 2. Optimal does not lie at the extremes. 3. Healthy people have stable blood sugars, but don’t necessarily get healthy by avoid carbs and protein and replacing that energy with refined fat. 4. You need to target the root cause (i.e. excess fat, which causes insulin resistance and metabolic syndrome) not the symptom (blood sugars). 5. The solution is high satiety nutrient dense foods and meals and managing meal timing by delaying your meals until your blood sugars return to below your baseline.
What about those that don’t carry excess fat that develop t2 diabetes or pre diabetes? Examples of endurance athletes that are lean developing this syndrome are abound.
The theory makes sense in some respects but I don’t think it’s the whole story.
Have a look a this post on the Personal Fat Threshold. Due to genetics and other factors, different people have varying abilities to store energy in their fat stores before it overflows back into their blood stream. https://optimisingnutrition.com/ted-naimans-dam-fat-storage-insulinographic-explained/
Interesting approach. All the keto-bashing puts me off, reads like click bait. I’ve never heard any authoritative proponent use the term “insulin toxicity”.
https://www.dietdoctor.com/insulin-toxicity-modern-diseases
agreed. real food will provide nutrients and satiety. insulin and pst meal blood sugars then look after themselves.
There were few things in the article that should have been cited. Also you cite basically two sources the diabetic doctor and a Facebook survey. Hardly random and highly subjective. I know your focus is not on type 1 diabetes treatment. I get that and honestly I learned a little something about insulin and how it relates to weight loss bmi etc. in your article. But as lifetime type 1 diabetic you have way over generalized your wife’s experience with diabetes treatment. Her personal experiences and yours are not necessarily the experience of most diabetics. For example my experience and those of the other 4 type 1 diabetics and 3 type 2 are very different. I have also been involved in a lot of clinical research and have spent hours talking to endocrinologists educators, researchers, and of course other type 1 diabetics in the studies. Not a single one of the many diabetics I’ve been around had every Endo doc and educator fail them like every single professional did your wife. If she experienced this everytime and the conversation always went you described(we both know this did not happen every time she talked to a professional about her diabetes), she is one of the most unlucky diabetics I have ever known. I’ve a lot of bad experiences too but the conversations I had with my doctors and team never went like that. Never. And that has not been the experience of the diabetics I have encountered. I’m not saying these experiences are the norm. But your wife’s experience should not be put out there like it is the norm either. If you had research(peer reviewed) that shows that please share. If your going to use science or even just critical thinking keep to that not hyperbole. Another example “CGM is painful and expensive.” We do pay too much for our medical care but CGM is not much more expensive than using test strips. This is especially true when you have to check multiple times daily. Dexcom for a lot of diabetics is about $50/month. Yes it’s expensive but it less expensive than going to the ER because of hypoglycemia. In the long term it could save money and your life, it did mine. Claiming it’s painful is irresponsible. The research on almost all of the CGM products show otherwise. This evidenced by how they market it to people who are tired of pricking their finger because of pain( I’m sure your wife would agree those finger pricks do not hurt). What pain you are referencing regarding CGM? . Many if not most experience no pain when placing new sensors. I have never heard anyone complain about pain when using CGM. I participated in three pre market clinical trials regarding CGM systems. Not a single person in all three of the trials complained of pain .I bet a simple Google confirmation bias search would find that most people do not complain about pain.
My point is if you’re going to use science stick to that and don’t make claims that are not supported by any research or data(peer reviewed if available).
Relating to stable blood sugars thanks to a pump and CGM technology my glucose levels have mostly stabilized recently and I feel so much better than I have for years. I’m exercising more as a result. Sure losing just a few pounds would be great but stable blood sugars have to be the primary focus for type 1s. Not to the exclusion of maintaining a healthy BMI.
That said and I mentioned earlier I did learn something from reading your article and I really appreciate that. I will be going and checking out your website too because I know I will learn something there .
Thanks for your response Keith.
You may find it useful to click on some of the blue underlined hyperlinks for some more information/references. Let me know if anything else needs to be referenced.
Maybe my window on the world from the Type 1 Grit community is jaded, but it appears to me that dietary advice fails many people with diabetes, particularly Type 1s.
I think CGMs are a Godsend for people with Type 1. We’re just getting AdnroidAPS closed-loop system working, and it’s a beautiful thing!
While I test my blood sugar frequently I haven’t worn a CGM myself. However, I do insert the Dex and Freestyle on my wife because she still finds it hard to do herself because of the pain at insertion.
In Australia, the cost of the Dex sensors is $90 per week plus a $540 transmitter. This is a lot of money for someone who doesn’t have T1D, particularly if it’s causing them to focus on the wrong numbers. https://amsldiabetesshop.com.au/collections/all
The point of the article though is that people who don’t have Type 1 can’t eat in a way that turns off their pancreas. The true way to reduce insulin across the whole day is to manage blood sugars BEFORE they eat. A lower-carb diet tends to be a lot more nutritious, but replacing carbs with refined fat does not lead to T2D reversal.
I don’t believe most people who just want to lose body fat need to go to the hassle and expense of a CGM, however, waiting until blood glucose drops before meals is an awesome biohack that has been shown to calibrate hunger signals that leads to true reversals of insulin resistance due to energy toxicity.
See https://optimisingnutrition.com/data-driven-fasting/ for more info.
I have worn FreeStyle Libre CGM for most of the last year and barely feel it when I attach it to the back of my upper arm. I don’t use the outside of the arm because I’ve accidentally knocked one off twice by bumping into something hard. The back of the arm is more protected and it’s also more fleshy, perhaps with fewer nerve endings. For me finger sticking stings for a good 30 seconds afterwards. CGM is great in comparison.
When I’m using Data-Driven Fasting I will take BGs on the skin on the outside of my arm a couple of times a day. Virtually painless and an order of magnitude cheaper.
The Glycemic Index is interesting. It measures the rise in BG after meals. The Food Insulin Index is more useful for people with Type 1 Diabetes as it measures the area under the curve insulin response to food. See https://optimisingnutrition.com/food-insulin-index-2/ for more details.
The problem with both of these though is that excessive focus on minimising insulin or blood sugar immediately after meals can lead to nutrient-poor low satiety foods. Conversely, if we focus on nutrient density and satiety and blood sugars before meals everything else that we’re aiming for falls into place (i.e. body composition, fat, insulin resistance, insulin levels across the whole day and BG rise after meals). SEe
https://optimisingnutrition.com/nutrient-density-101/
https://optimisingnutrition.com/calculating-satiety/
https://optimisingnutrition.com/how-does-protein-suppress-your-appetite/
Which part are you objecting to in particular? Any specific feedback would be welcome. Did you read this bit “If you are part of the 1 in 8000 people with T1D whose pancreas doesn’t work, stabilising your blood sugars and insulin should be your #1 priority!”
The T1Ds I know with the best HbA1cs follow Bernstein’s Law of Small Numbers. See https://pubmed.ncbi.nlm.nih.gov/29735574/
thanks for sharing your insights.
I’m curious about one thing. Why balanced diet based on low glycemic index food not mentioned?
Because low GI means lower insuline release so stable blood sugar. To complete your example, coconut sugar has the same IG as milk.
I want to know if smoking cigarette is or not for the people who suffering diabetes
I’m not aware of any correlation between diabetes and smoking. Smoking is not ideal for other health reasons (e.g. lung cancer).
It is easy to concur with Dr. Naiman.
One motto from Peter from Hyperlipid seems to fit to your thinking as well: “the main task for insulin is to stop lipolysis”.
For people slowly depeloping t2d, the blood glucose hyper-ride seems to be the very last red flag? Insulin excursions short term a’la Kraft would allow early intervention… The concept you bring up, all day insulin levels and pre-meal glucose, this is new and interesting.
Insulin speeds up the glucose uptake into cells, but there are GLUTs available for slow removal. I guess your family has firsthand experience on this, is the rate of disappearance less than GNG in the liver?
Insulin sensitivity and gaining fat (weight) is also interesting. The visceral fat seems to be 4 times metabolicly more active than subcutateous fat (meaning more sensitive). This would implicate chronicly higher (peaks and duration, eventually all-time) insulin levels to store effectively fat into visceral areas? is this your understanging, or…?
McLaughlin did further analysis of DietFits trial, and found interesting differences within goups. Invisible at first, the lower carb group could dimish the size of the adipose cells. This allows more flexibility and capasity within the cells…
https://www.healio.com/news/endocrinology/20191205/despite-similar-weight-loss-lowcarbohydrate-diet-delivers-insulin-reductions-smaller-fat-cells-than
The topics that did not appear in here: vLDL i.e. triglycerides can be used as energy, affecting the total energy content in blood ? Also, the omega-6 fats can behave like turbocharged glucose, filling up cells very effectively. Compare to sat fats, whose burning signals energy satiaty by ROS, creating transient insulin resistance (Peter and dr. Eades). Your take on these?
rgds JR
Thanks for your detailed and thoughtful response. I really appreciate it. Thoughts.
– It’s always easy to concur with Ted. It’s nice to have him as an advisor to so we keep on the straight and narrow.
– Kraft is certainly interesting and useful, but apparently impractical/expensive as a one-off test, let alone as a tool to track progress regularly. Waking glucose, BG before meal and waist to height seems to be a much more useful way for the average enthusiast to keep track.
– All-day total insulin is only really possible to track if you have your pancreas in your pocket and you can see the digital readout (i.e. insulin pump for T1Ds).
– Insulin “pushing” glucose into the cells should ideally be an emergency function of insulin when glucose is high. Before our creation of agriculture with constant food availability, non-insulin mediated glucose update (GLUT4) would have been the “normal” mechanism when there was not a constant oversupply of energy.
– Adipose tissue seems to be “well designed” for storage of any excess energy. It’s only when that becomes full that we need to ramp up insulin production to jam the extra energy into our vital organs.
– Fascinating analysis of DIETFITS! When we focus on nutrient density and satiety we tend to get less non-fibre carbohydrates (i.e. lower carb, but not high fat). See https://optimisingnutrition.com/analysis-of-optimising-nutrition-recipe-series-22-books/
– Omega 6 fats seem to produce a greater endocannabinoid response which drives appetite. As a general rule fat is less satiating, however, omega 3 and cholesterol seem to have positive impacts on satiety. Omega 6 drive overconsumption. Saturated fat is sort of in the middle. Seems if it’s an ingredient with other fats then the satiety response is not high, but when it’s mainly sat fat with protein (and less omega 6) it has a beneficial effect on satiety. https://optimisingnutrition.com/which-fats-will-make-you-skinny/
i can’t tell if this is in line with Ben Bikmans work or if he is part of the insulinphobic group. He speaks a lot of glucagon and the role of the two different fats as you discussed. Marty answer as well please?
I’m definitely in line with Ted’s thinking on pretty much everything. I wouldn’t call myself insulin phobic. I’m think we need a better understand if what actually affects insulin and leads to improved body composition.
Thanks. Great article.
thanks for reading!
And what if after eating a small fruit the sugar is high and at the same time we are very hungry again?
You don’t NEED to eat because your glucose fuel tank is still full. However, it should not take long for glucose and insulin to decrease again compare to a large carb+fat meal.
I have found since lifting weights fasted in the morning and coming home to some lean protein and just the right amount of carbs,I am feeling much better,and I can tell my metabolism is a little better..I will continue to eat after fasting (which has become a lifestyle for me now) I am just not that hungry anymore.
resistance training + lean protein seems to work really well for most people.