Embark on a journey to metabolic excellence as you discover how blood glucose levels unveil the roadmap to dietary success.
This section of the Macros MAsterclass FAQs steps you through the impact of carbs on blood sugar and how nuanced dietary adjustments can herald remarkable health transformations.
- Do I Need to Test My Blood Glucose?
- How Does Nutrient Optimiser Use the Blood Glucose Data?
- How Often Will I Need to Test My Blood Sugars?
- What Glucose Meter Do You Recommend?
- Would a Continuous Glucose Monitor (CGM) Be Better?
- What are the official limits for Type 2 diabetes and prediabetes?
- How Do Carbohydrates Affect My Blood Sugars?
- How Does Fat Affect My Blood Sugar?
- Does Insulin Resistance Make It Harder for Me to Lose Weight?
- Why Is My Waking Blood Sugar the Highest?
- How Much Should My Blood Glucose Rise After a Meal?
- Should I Eat Less Protein if I Have Diabetes?
- When Should I Test My Blood Glucose After Eating?
- What is a Healthy Waking Glucose Level?
- How Can I Optimise My Insulin Dosing Regime?
- How to Accurately Count Carbohydrates for Insulin Dosing
- How Can I Make Blood Glucose Testing Easier?
- More
Do I Need to Test My Blood Glucose?
Testing your blood glucose is an optional tool used in the Macros Masterclass to help find your carb tolerance.
Understanding your blood glucose response to what you currently eat can be beneficial for people who:
- are managing diabetes (Type 1 or Type 2),
- know they have prediabetes or
- have a family history of diabetes.
It can also be helpful for people following a low-carb or keto diet to get a better idea of how much they need to restrict their carbohydrate intake. However, decreasing carbohydrates more than necessary can be counter-productive, especially if it leads to replacing nutrient-dense foods with excessive dietary fat.
How Does Nutrient Optimiser Use the Blood Glucose Data?
Nutrient Optimiser will lower your carbohydrate target if your blood sugars rise by more than 1.6 mmol/L or 30 mg/dL after you eat. This response indicates you are overfilling your glucose fuel tank in your body.
If you find that your blood sugars are already in the healthy range, you can get on with focusing on nutritious, high-satiety foods without worrying about limiting your carbohydrate intake.
The reality is that nutrient-dense, high-satiety foods tend to be low in refined carbohydrates that will raise your blood sugars anyway.
How Often Will I Need to Test My Blood Sugars?
If you decide to test your blood sugars, we recommend taking measurements before and after most of your meals during the first baselining week. However, you don’t have to continue testing if your blood glucose levels are consistently in the healthy range.
Instead, you can focus on dialling in your macronutrients for the rest of the Macros Masterclass. If you want to see how much your blood sugars have improved, you can restart testing towards the end of the Masterclass.
What Glucose Meter Do You Recommend?
You can use any blood glucose meter for the Masterclass. However, the Contour Next One meter tends to be the best in terms of accuracy and features. They can be purchased online or from your local chemist.
Would a Continuous Glucose Monitor (CGM) Be Better?
You can use a CGM if you already have one. However, we don’t recommend buying one specifically for the Macros Masterclass because CGMs tend to provide too much data for some people to make sense of. This often leads people to avoid carbs (and sometimes even protein) in favour of excessive amounts of low-satiety, nutrient-poor dietary fat.
For more details, see:
- Want To Lose Fat? DON’T Target Stable Blood Sugars! (Why your CGM could be making you fat), and
- How to Make the Most of Your Continuous Glucose Monitor (CGM) Data.
What are the official limits for Type 2 diabetes and prediabetes?
Your doctor will diagnose you with prediabetes if you have an HbA1c greater than 6.0% and Type 2 Diabetes once your HbA1c hits 6.5% and above. Official cut-offs for blood sugar blood and HBA1c are shown in the table below.
Note: To convert between mg/dL (US units) and mmol/L (imperial units used by the rest of the world) or divide or multiply by 18.
How Do Carbohydrates Affect My Blood Sugars?
Achieving healthy blood glucose levels is a critical part of our programs. Elevated blood glucose is a strong indicator of metabolic diseases and associated conditions such as heart disease, cancer, and diabetes.
In the Macros Masterclass, you will use your blood glucose levels to dial in your carbohydrate intake to achieve healthy blood glucose variability. A rise in blood glucose of more than 30 mg/dL (1.6 mmol/L) indicates you are overfilling your glucose fuel tank or the glucose in your blood and the stored glycogen in your liver.
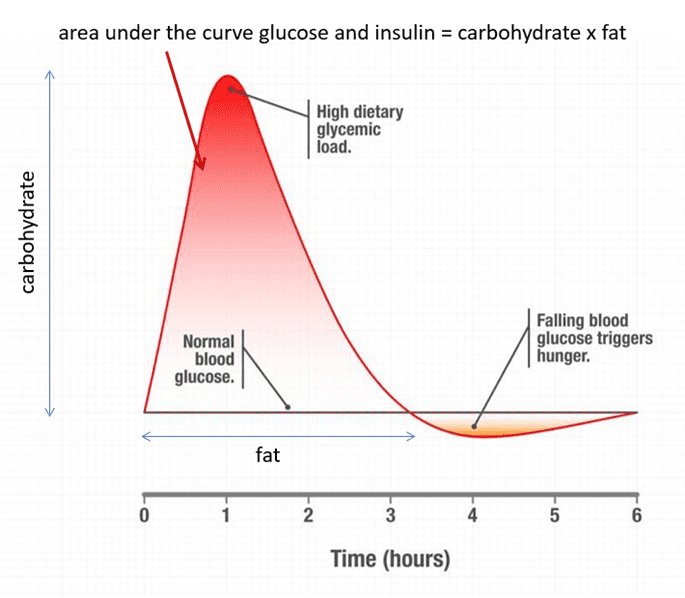
Carbohydrates will raise your blood sugar levels quickly. Your pancreas raises your insulin levels to abruptly shut off the release of stored energy, enabling you to burn off the excess glucose in your blood from the food you just ate.
The problem with excess refined carbs for many people occurs when their blood sugar levels come crashing below what is normal. At this point, you are more likely to feel excessively hungry and make poorer food choices to raise your blood glucose levels quickly.
It’s not that the increase in insulin caused by the carbs drives you to store more energy, but rather that the blood sugar crash that can occur drives people to overeat and more insulin is subsequently required to keep the extra energy in storage.
Nutrient Optimiser will guide you through finding the carbohydrate intake that works best for you. This will help you avoid excessive rises in glucose that lead to crashes after eating, driving you to make poorer food choices.
The Smart Macros algorithm in Nutrient Optimiser will guide you to slowly titrate your carbohydrate target each week until you can achieve stable blood glucose levels or rise less than 30 mg/dL (1.6 mmol/L) after meals.
Once your blood glucose is consistently in the healthy range, you don’t need to worry about dialling back carbohydrates further. Flatline blood sugars can be achieved with high-fat diets with minimal carbs and protein. But this is typically a less satiating and nutritious way of eating. Hence, we don’t recommend unnecessarily decreasing carbs beyond what is required to achieve healthy blood sugar variation.
How Does Fat Affect My Blood Sugar?
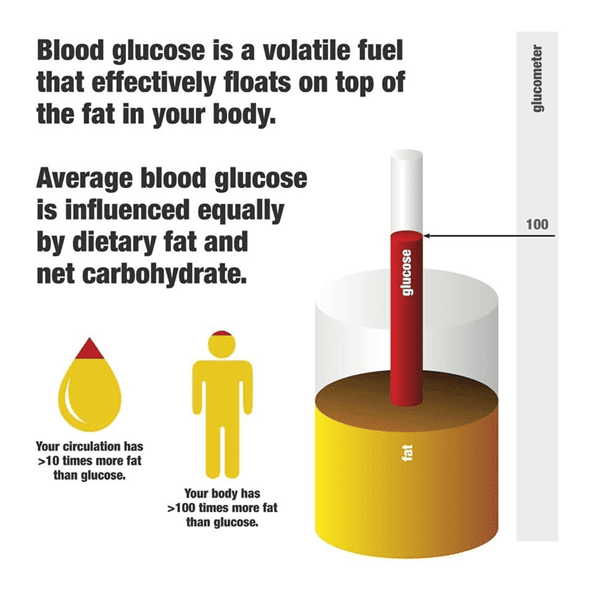
While carbohydrates increase your blood sugars over the short term, dietary fat provides more stable blood sugars that rise slightly over the long term.
Our Data-Driven Fasting guides participants to wait to eat until their blood sugars return to below baseline before eating again. While high-fat meals don’t tend to raise glucose much, they do meals that prevent your blood sugars from falling. Glucose effectively ‘backs up in your system’ while your body uses up the excess dietary fat.
Rather than worrying about achieving flatline blood glucose levels, it’s better to focus on reducing the area under the curve of your glucose response. You can think of the area under the curve of your glucose and insulin response to the food you eat as proportional to the fat and carbs you consume in each meal.
When combined, fat and carbs will keep your blood sugar and insulin elevated for longer. So, if you want to eat less, focusing on keeping fat or carbs lower at each meal is ideal.
A nutrient-dense, protein-focused diet that contains less energy from fat and carbs will enable you to tap into stored energy again sooner while still providing the required nutrients.
Does Insulin Resistance Make It Harder for Me to Lose Weight?
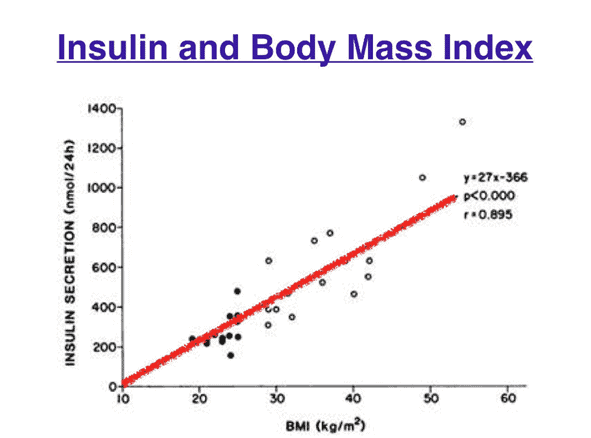
There is a common misconception that being insulin-resistant or having Type-2 Diabetes makes it harder to lose weight. However, the opposite is true.
We become insulin resistant because we are obese. We are not obese because we are insulin resistant. As shown in the chart below, if you carry more body fat, your body will need to produce more insulin throughout the day to store your stored energy. This distinction and a proper understanding of the cause-and-effect relationship is critical!
People who can gain massive amounts of weight are often highly insulin-sensitive. Despite having higher body fat levels, they usually have normal blood glucose levels before developing diabetes.
Lean people are typically much more insulin-sensitive, meaning they can quickly gain muscle or fat when they eat. However, weight loss generally slows as someone becomes leaner, and hunger increases to prevent starvation.
It takes a massive amount of discipline and self-restraint for bodybuilders to diet down for a bodybuilding show. However, many of them end up regaining the weight they shed extremely quickly afterwards from a massive appetite upregulation after pushing their body to the extremes.
Someone who is obese is more likely to be insulin resistant and have elevated blood glucose levels and excess energy overflowing into their bloodstream. However, it’s hard for them to gain more body fat because their adipose tissue is already full. Once they drain the excess energy from their bloodstream, they can lose body fat. Their pancreas is likely struggling to continue producing enough insulin to keep their extra energy in storage. As they lose body fat, their insulin levels will reduce, and they will become more sensitive to the effects of insulin.
For more details on the role of insulin in your body, see:
- How to Reverse Your Insulin Resistance,
- What Does Insulin Do in Your Body?
- Personal Fat Threshold Model of Insulin Resistance, Diabetes and Obesity
Why Is My Waking Blood Sugar the Highest?
If you have plenty of stored body fat, your body will release that stored energy overnight into your bloodstream.
Your body can make glucose from protein and the glycerol backbone of dietary fatty acids. So, if you have excess energy stored in your body, the glucose will back up in your system and overflow into your blood.
Making sure you are not overeating too late may help decrease waking blood sugars, but it may take some time until you can reduce your body fat levels to more optimal levels.
How Much Should My Blood Glucose Rise After a Meal?
If you see your blood glucose rise by more than 1.6 mmol/L (30 mg/dL) one to two hours after you eat, it likely means that you ate too much or too many carbohydrates at that meal. You should either avoid that meal or eat less of it in the future. Your glucose tank is full, so you don’t need more carbs.
Many people find their blood glucose rises more after dinner, which indicates their energy stores are overfilled. As a result, they may benefit from reducing the size of their dinner and prioritising larger meals earlier in the day when their energy tanks are more depleted.
The rise in glucose after you eat is more of a reflection of what you ate. On the contrary, your fasting blood glucose and glucose before meals indicate your metabolic health and whether you are over-fuelling throughout the day.
Most people don’t need to be too concerned about their post-meal blood glucose if they focus on nutrient-dense whole foods, which typically don’t contain refined grains or added sugars.
Should I Eat Less Protein if I Have Diabetes?
Some people mistakenly aim for perfectly flatlined blood glucose by reducing protein and carbohydrates. Unfortunately, this often ends in overeating low-satiety, nutrient-poor, high-fat foods, which leads to increased energy intake, weight gain, and insulin resistance!
If you are insulin resistant or have elevated blood glucose, there will be more dietary protein ‘lost’ in its conversion to glucose through gluconeogenesis and less available for muscle protein synthesis. To make up for the protein lost to glucose, your appetite will increase. Thus, you will consume extra energy to get the protein you need.
For this reason, it is critical that people with Type-2 Diabetes, prediabetes, or any degree of insulin resistance emphasise higher protein percentage foods and meals (rather than avoiding it) until they lose their excess body fat, reduce blood glucose levels and inherently become more insulin sensitive.
When Should I Test My Blood Glucose After Eating?
The rate your blood glucose rises and falls after a meal depends on your eating and your unique metabolism. For example, blood glucose rises quickly after a high-carb, low-fat meal (as represented with a green line in the chart below). In contrast, blood glucose will increase more slowly after a high-fat meal (as shown in the red line in the chart below).
Testing one hour after you finish eating is a good rule of thumb. If you’re curious, you could also do extra testing every half hour for two or three hours after a couple of meals to find out when your glucose levels peak. If you typically consume a lower-carb diet, you may find your glucose peaks two hours after you finish eating.
If you find your glucose peaks at two hours rather than one hour, you can simply test your post-meal glucose two hours after eating. You don’t need to stress about being too precise for our purposes in the Macros Masterclass.
What is a Healthy Waking Glucose Level?
While most of us focus on total weight and body fat, being below your Personal Fat Threshold is arguably a more important measure of your metabolic health.
But how do you know if you are below your Personal Fat Threshold?
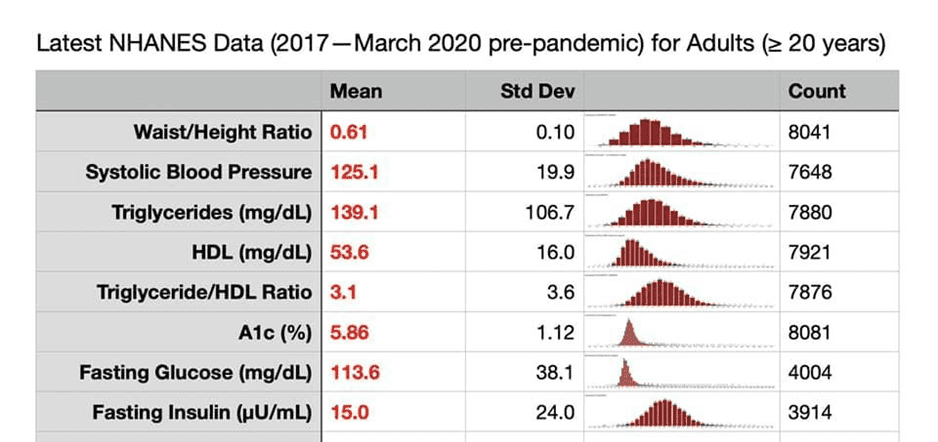
As shown below, the latest US NHANES data indicate that the average waking (fasting) glucose level is 114 mg/dL or 6.3 mmol/L.
However, as shown in the chart below (from Association between fasting glucose and all-cause mortality), the lowest risk of dying from any cause aligns with a fasting glucose between 70 and 100 mg/dL (4.4 to 5.6 mmol/L).
If your waking blood glucose is in the optimal range, it means:
- you are insulin sensitive,
- your insulin levels are low,
- your body fat can absorb extra energy from your food, and
- you do not have excess energy backing up into your bloodstream.
You can track your waking glucose in Nutrient Optimiser. You should be aware that your waking glucose may increase initially as insulin drops, the stored energy is released, and you start to lose weight. Later, you may see your waking glucose stabilise at a lower level when you stop losing weight.
How Can I Optimise My Insulin Dosing Regime?
While we can’t help you adjust your medication if you inject insulin to manage Type-1 or Type-2 diabetes, knowing your carbohydrate intake at each meal can be a helpful tool to dose insulin more accurately.
As you dial back your carbohydrates, you should be mindful that you will require less bolus insulin at meals. In addition, as you lose weight and become more insulin sensitive, you will need less long-acting basal insulin.
You should work with your healthcare team to scale back your medications as your metabolic health improves. We love it when people can ditch their medications after following our programs!
How to Accurately Count Carbohydrates for Insulin Dosing
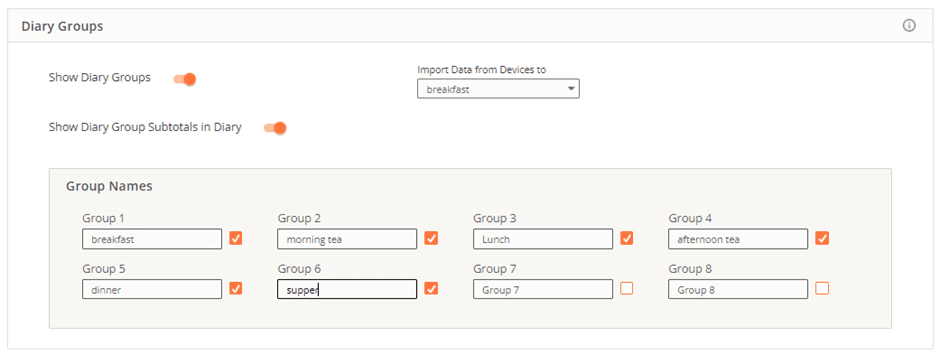
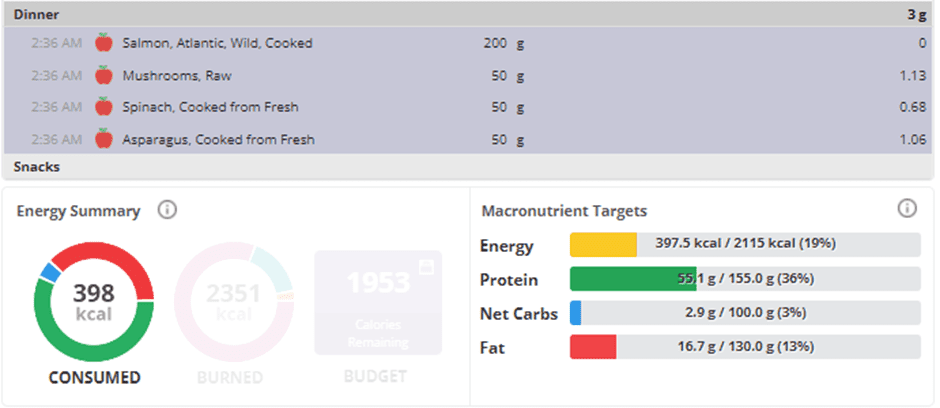
If you have the Gold version of Cronometer, you can set up diary groups for each meal and snack.
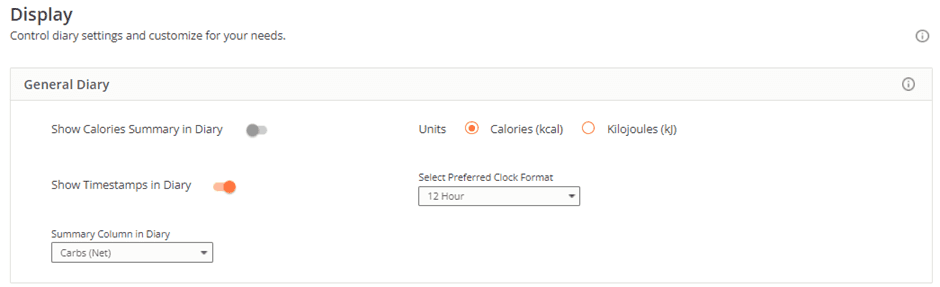
Select ‘net carbs’ to display in your diary for each meal or snack under settings -> display on the web interface.
On the app version of Cronometer, you can select ‘show macronutrient breakdown’ to show the carbs, fat, and protein from each meal in the daily diary.
You can use this information to calculate your insulin dose precisely to account for the non-fibre carbohydrates you consume at each meal.
If you don’t have the Gold version of Cronometer, you can simply select the ingredients that make up the meal. The energy summary area below will show the macro breakdown for the selected ingredients.
During the Macros Masterclass, the Smart Macros algorithm in Nutrient Optimiser will guide you through dialling back your carbohydrates until you achieve healthy blood sugar variability or a rise of less than 30 mg/dL (or 1.6 mmol/L) in blood sugar following a meal.
How Can I Make Blood Glucose Testing Easier?
Here are a few tips if you are new to blood sugar testing:
- While most people use their fingertips to test blood sugar, they can be very sensitive. You can get blood from less sensitive locations, including the sides of your finger or the outside of your forearm. You may get slightly different values when testing on other fingers or parts of your body. This is not an issue, so long as you are consistent with where you test.
- Make sure you have a sharp lancet, as they hurt less. You don’t have to change it all the time, but try a new lancet if you feel it’s hurting more than usual. They get blunt after a few weeks.
- Meters like the Contour Next One allow you to add more blood if you don’t get enough the first time to avoid wasting a strip.
- You only need enough blood to get a test result, so dial back the lancet depth to one that minimises discomfort but still draws enough blood.
- Ensure you don’t have food or dirt on your fingers when you test.
- It helps if you have warm hands and are well hydrated. You can try shaking your hands or running them under warm water for a few seconds to bring more blood to your fingers first.
- Before you prick yourself, it’s a good idea to rub your skin a little to mobilise the blood. This allows you to have a lower setting on your lancet and hopefully less discomfort.
- If you get a blood glucose reading significantly different from what you expected, you can retest again. After that, just accept it and move on.
- If you don’t initially get enough blood to take a test, you can push down again with the lancing device without pricking again. The pressures will give you a little bit more blood.







Thanks for sending this, Marty. I only just saw this article in read it. My blood glucose level is my main concern. I have not been testing regularly the last 4 days. Should I start over with Day 1 and test my blood sugar before and after each meal so that I can get an accurate image of my blood glucose level? How do I do that?
you could always start now by testing before and 2 hours after meals to see how you respond to the food you eat. but starting 8 Jan we’ll guide you through the process of adjusting your diet to optimise your blood glucose levels.
you can join at https://app.optimisingnutrition.com/data-driven-macros
Hi, I think this is a basic question I should know but how do I figure out my “trigger,” which I think is the point at which I am hungry enough to eat my next meal. I see “trigger” on NO under Progress, then Biomarkers, then Pre-meal glucose, but I can’t understand how to read it. thanks!
in the DDF challenges, we use the DDF app to calculate the average premeal trigger during the baselining period. the app then lower the trigger based on progress through the challenge.