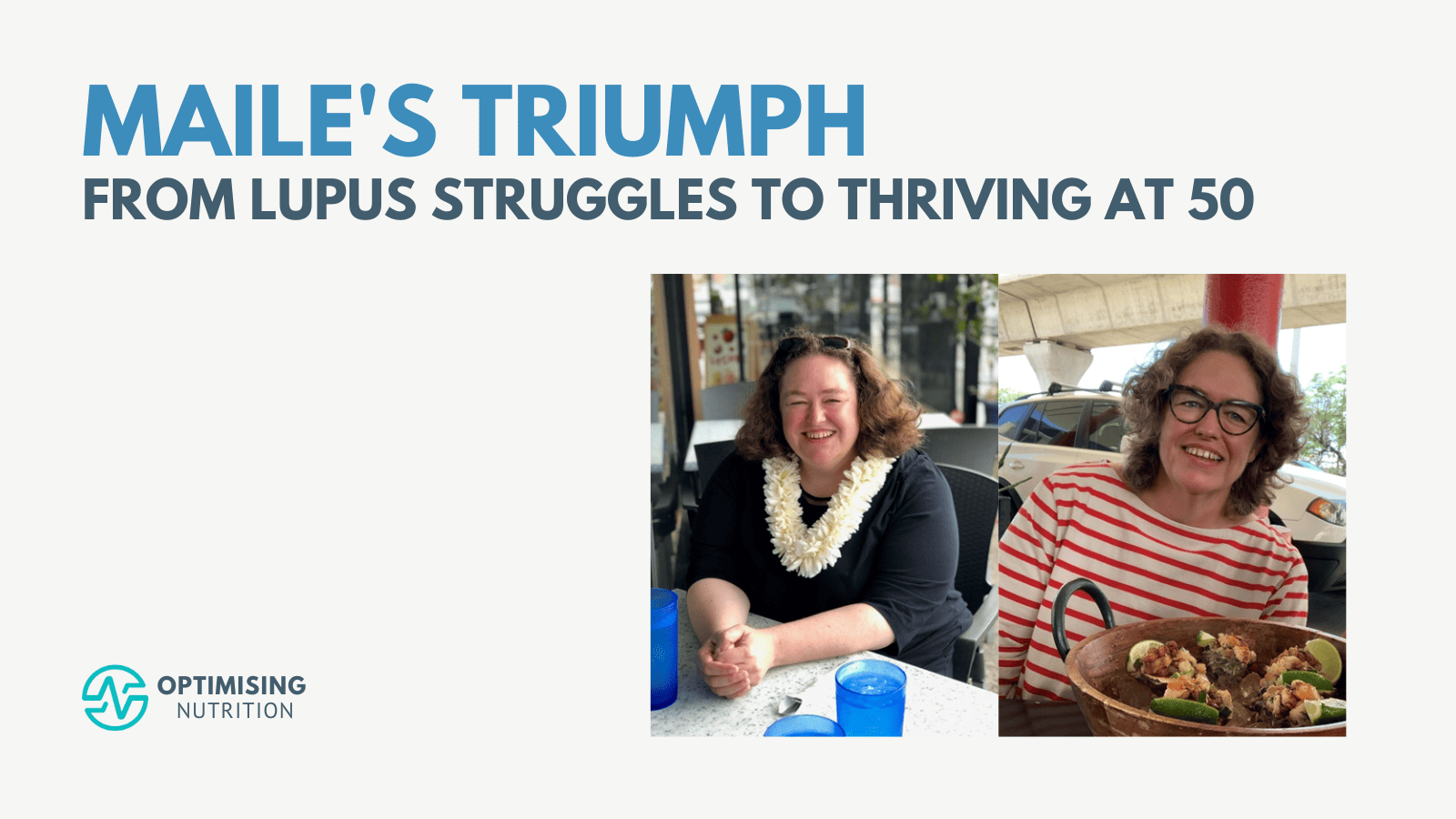
Maile’s Triumph: From Lupus Struggles to Thriving at 50
I’m excited and honoured to share Maile’s story of nutritional optimisation. Maile first caught our attention when she topped the weight loss leaderboard in our August 2023 Data-Driven Fasting Challenge with a massive 15 lb (6.8 kg) in just four weeks. She then returned in our Macros Masterclass and Micros Masterclass to optimise her diet … Read more