The ‘Dawn Phenomenon’ refers to early morning blood sugar spikes, a common yet perplexing occurrence, especially among people with diabetes. Understanding the normal morning rise in blood glucose range helps individuals better manage their blood sugar levels.
While some dawn effect is normal, managing it before it gets out of control is crucial. In this article, we’ll show you how to reverse the dawn phenomenon naturally. This guide also explores the link between fasting blood sugar and the dawn phenomenon, providing actionable insights to control and maintain healthy blood sugar levels.
- What Is the Dawn Phenomenon?
- Why Does Dawn Phenomenon Occur?
- Is Dawn Phenomenon Normal?
- What are Normal Waking Glucose Levels?
- What Does the Dawn Phenomenon Feel Like?
- Should I Worry About Dawn Phenomenon?
- How Many Hours Does Dawn Phenomenon Last?
- Do All Diabetics Have Dawn Phenomenon?
- Can Stress Cause Dawn Phenomenon?
- How Do You Get Rid of the Dawn Phenomenon?
- Addressing Energy Toxicity
What Is the Dawn Phenomenon?
The dawn phenomenon simply explains the occurrence of high blood sugars—usually exceeding your blood sugar target—in the early morning hours.
Why Does Dawn Phenomenon Occur?
The short version
Dawn phenomenon occurs due to a surge of hormones early in the morning, typically between 2 and 8 a.m.
This leads to a rise in your blood glucose levels, so you’re fuelled up and ready to start the day.
The Detailed Version
Your body has an internal clock that functions like a self-timer system. Here, it releases hormones, neurotransmitters, and bodily substances at similar times every day. This ‘clock’ is known as your circadian rhythm.
Your circadian rhythm is closely tied to your eating, sleeping, waking, activity, and light exposure; your body uses your day-to-day interactions with the world around you to set this biological clock.
As your body prepares to wake, melatonin lowers, and growth hormone, cortisol, epinephrine, and adrenaline naturally rise.
This hormonal cascade also triggers the release of the hormone glucagon from your pancreas, catalyses the breakdown of stored glycogen in your liver and increases the glucose in your bloodstream.
Viola! You are fully fuelled, energised, and ready to bounce out of bed to start the day.
Is Dawn Phenomenon Normal?
Some level of dawn phenomenon is perfectly normal, even in someone who is metabolically healthy. However, people with insulin resistance or diabetes (either Type 1 or Type 2) tend to see a higher rise in the morning.
In several previous articles, we’ve discussed how glucagon is the accelerator for your metabolism, while insulin acts like a brake. In metabolically healthy people, insulin is also released to balance glycogen. Hence, their blood glucose doesn’t rise too much.
Type 1 Diabetes
From people with Type-1 Diabetes, we know that insulin levels are the lowest overnight. However, the liver pushes out glucose a few hours before waking.
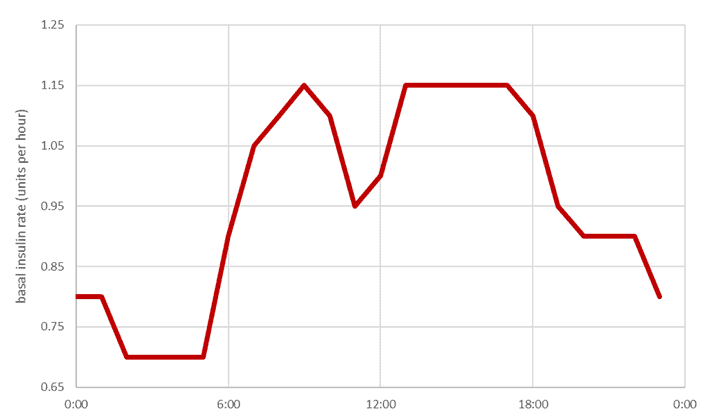
The chart below shows my wife Monica’s basal insulin rates across the day. This basal insulin is required to keep her glucose in the normal healthy range, even if she doesn’t eat.
- After she eats her evening meal, insulin is at its highest as she metabolises and stores it.
- Conversely, her insulin and blood glucose are lowest through the early morning hours between 2 and 5 a.m.
- Then, as her body prepares to wake, glucose and insulin rise. Without this rise in insulin, her waking glucose would be much higher, even without eating.
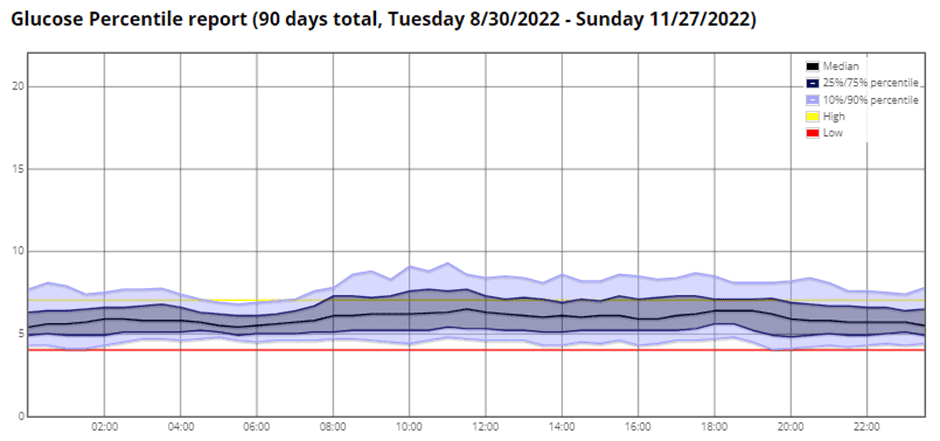
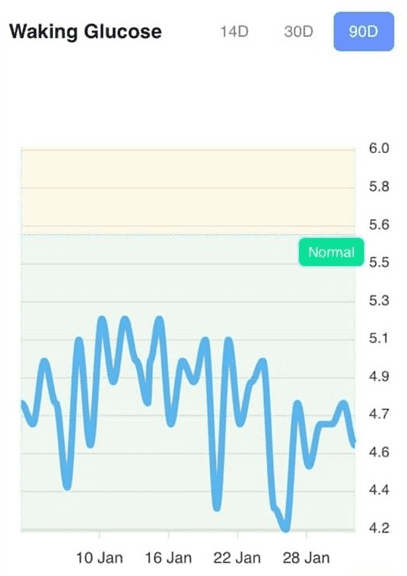
For reference, the chart below shows her glucose over three months. Notice how it is lowest around 6 a.m. and then rises through the morning.
Insulin Resistance & Type 2 Diabetes
Interestingly, we see a glitch in the matrix when someone has some degree of insulin resistance or cannot produce adequate insulin due to insulin resistance.
While some rise in glucose in the morning is normal, someone who is insulin resistant has an imbalance between glucagon and insulin. Because they are insulin resistant, insulin cannot do its job properly to keep glucose in the normal range.
As we’ll discuss later, energy toxicity is the root cause of insulin resistance. Because your body holds too much stored energy, insulin can’t do its job properly to hold all the energy in storage and balance the normal morning glucagon response. For more details, see What Is Insulin Resistance (and How to Reverse It)?
Eating Too Late
It’s also worth mentioning that eating too late can also keep blood sugars high. It makes sense that the later you stop eating, the higher your waking glucose will be. So closing the kitchen a little earlier is a practical short-term hack to lower your waking glucose.
What are Normal Waking Glucose Levels?
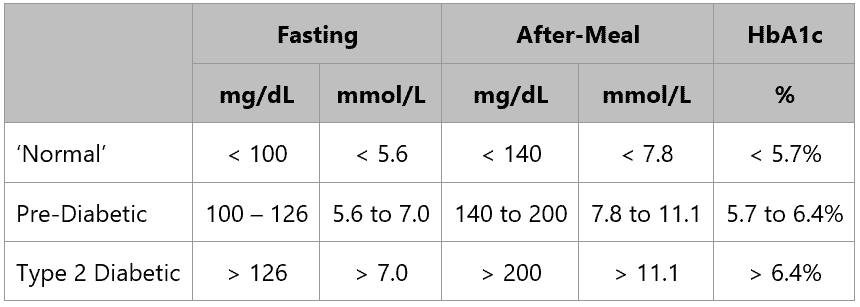
The table below shows the generally accepted cut-off levels for normal waking glucose levels.
- If your waking glucose is less than 100 mg/dL or 5.6 mmol/L, then you’re likely metabolically healthy and insulin sensitive,
- A waking glucose of 100 to 126 mg/dL (or 5.6 to 7.0 mmol/L) indicates you are in the pre-diabetic range, and
- A waking glucose of 126 mg/dL or 7.0 mmol/L is one of the indicators of Type 2 Diabetes.
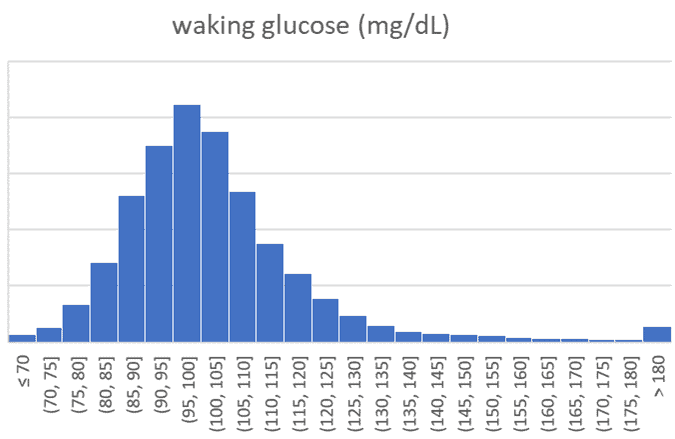
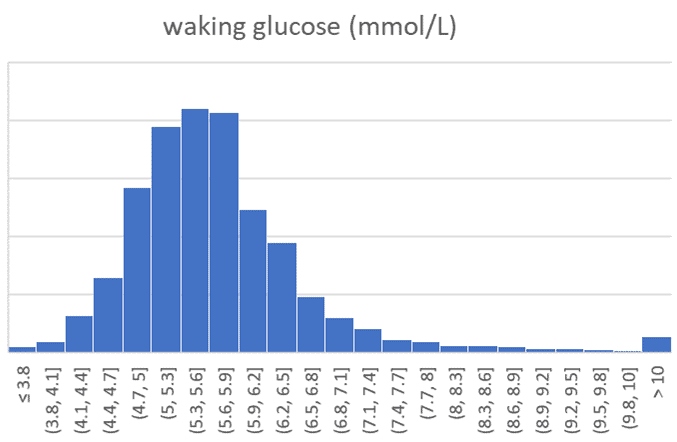
The charts below show the range of 124,858 waking glucose values that have been entered into the Data-Driven Fasting app over the past few years.
The table below summarises this data and shows an average waking glucose of 103 mg/dL (5.7 mmol/L).
| mg/dL | mmol/L | |
| Average | 103 | 5.7 |
| 15th | 88 | 4.9 |
| 85th | 116 | 6.4 |
| n | 124,858 | 124,858 |
While your waking glucose can be tricky to control, it’s potentially the most important to manage. Fasting glucose is a powerful indicator of your metabolic health. As the chart below from Jee-Jeon et al., 2017 shows, a fasting glucose level between 80 and 100 mg/dL tends to align with the lowest hazard ratio or risk of dying from any cause (all-cause mortality).
What Does the Dawn Phenomenon Feel Like?
Everyone experiences the dawn phenomenon differently.
Some people may feel no symptoms, while others may experience symptoms such as:
- a rapid heartbeat,
- sweating,
- anxiety, or
- shakiness.
Others may experience fatigue, increased thirst, and weakness.
The best way to understand if you’re experiencing Dawn Phenomenon is to get a simple glucometer and test your glucose when you wake up for a few days. There’s no need to wait until your next doctor visit for a blood test.

Should I Worry About Dawn Phenomenon?
There is no need to worry about a small rise in your blood glucose in the morning, as it is a regular occurrence—to some degree.
As with anything, the severity and intensity of your blood sugar readings and other symptoms matter. If you have blood sugars that could be considered hyperglycaemic upon rising or an increased Hb1Ac, it might be worthwhile to talk to your doctor.
Additionally, if you show other symptoms of high blood sugar, like:
- Increased thirst,
- Dry mouth,
- Frequent urination,
- Fatigue,
- Blurred vision,
- Nausea,
- Gastrointestinal discomfort,
- Weight loss or weight gain,
- Mood swings,
- Recurrent infections,
- Depression,
- Anxiety, or
- High blood sugar readings,
This should warrant further investigation into your metabolic health.
While the dawn phenomenon is not abnormal in and of itself, coinciding symptoms and amplified glucose readings might point to deeper dysfunction, like insulin resistance or Type-2 Diabetes.
How Many Hours Does Dawn Phenomenon Last?
The dawn phenomenon typically lasts for two to three hours. If you are more active in the morning, you can expect it to ‘wear off’ sooner. Going for a morning walk or exercising before your first meal is a great way to burn off the excess energy in your system. Conversely, it might hang around for longer if you are less active.
Do All Diabetics Have Dawn Phenomenon?
The dawn phenomenon is a regular occurrence that is a product of human physiology and the body’s natural circadian rhythm. Hence, most people—even those free of metabolic syndrome—experience it to some degree.
However, it is often amplified in someone with metabolic syndrome and diabetes, and their blood sugar is more likely to reach hyperglycaemic levels. While someone with diabetes might be more likely to see their sugars stay high after waking—especially if they have known insulin resistance—it is unique to the individual. That said, it’s estimated that around 50% of people with T1D and T2D experience the dawn phenomenon.
Can Stress Cause Dawn Phenomenon?
The dawn phenomenon is a normal physiological process in the early morning hours due to the body’s natural sleep-wake cycle. Thus, stress does not directly cause the dawn phenomenon.
However, while stress does not cause the dawn phenomenon, stress can also raise blood sugar.
When stressed, your body releases hormones like epinephrine and norepinephrine in the short term and cortisol over the long term. All three substances work synergistically with glucagon and trigger its release.
This results in the release of stored energy from liver glycogen, body fat, and sometimes even your muscles, depending on how much energy your body needs. Hence, you may see your blood glucose rise more if stressed. Elevated waking glucose can indicate that you’re stressed or getting sick and need to invest in a little more self-care and rest.
An example of the relationship between stress and blood sugar is going to the gym. Exercise—even one that you’re willingly choosing to do—is a stressor. Hence, many people who track their blood glucose report seeing their blood glucose rise during and immediately after their workout.
How Do You Get Rid of the Dawn Phenomenon?
There is no short-term ‘cure’ for the dawn phenomenon, but there are ways to control it, depending on your situation and circumstances.
If you have Type-1 Diabetes or insulin-dependent Type-2 Diabetes, you can try increasing your night-time insulin to lower your waking glucose.
If you take blood glucose-lowering medications, you can experiment with the time you take them. For example, if you take them in the morning or before meals, you may try taking them after or later in the day.
Aside from directly intervening to manage the symptoms, there are several things you can do to address the root cause of the insulin resistance that’s making your body unable to control your blood sugars and regulate insulin levels: energy toxicity.
Addressing Energy Toxicity
Many people believe that diabetes and insulin resistance results from insulin toxicity.
However, your body is incredibly efficient and does not produce more insulin than required to hold your stored energy in storage (unless you have an insulinoma or a pancreas tumour).
If you are insulin resistant and have high waking glucose levels, you have likely exceeded your Personal Fat Threshold or the amount of energy your body can comfortably store without overflowing into your bloodstream.
The key to relieving your body of energy toxicity—the root cause of metabolic syndrome, Type-2 Diabetes, pre-diabetes, and related conditions—is to drain the excess energy you have stored on board.
You can begin to do this by not eating the first thing you wake up if your blood glucose is high in the morning, especially if you are not hungry. When you start feeling hungry, you might opt for a higher-protein meal. If you are hungry and your glucose is high, you know you have plenty of fuel onboard and only need protein and nutrients.
Prioritising protein earlier in the day often causes blood glucose to fall, and you can eat again sooner rather than waiting all day. This is because the body requires insulin to utilise protein, but protein does not raise blood sugar significantly.
Prioritising a higher protein meal first up is a common ‘hack’ that people in our Data-Driven Fasting Challenges use to feel full while also dropping their blood glucose levels.
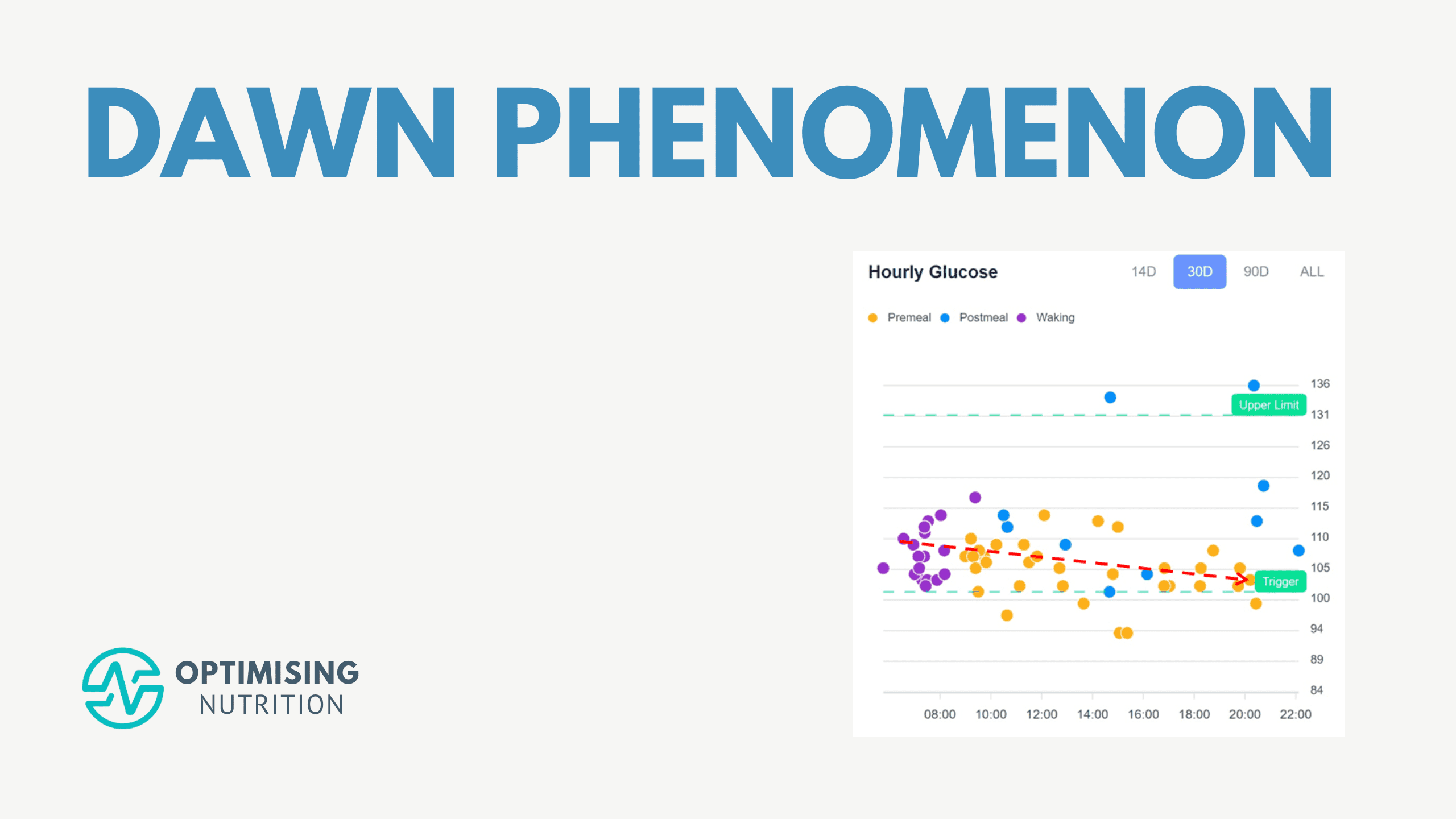
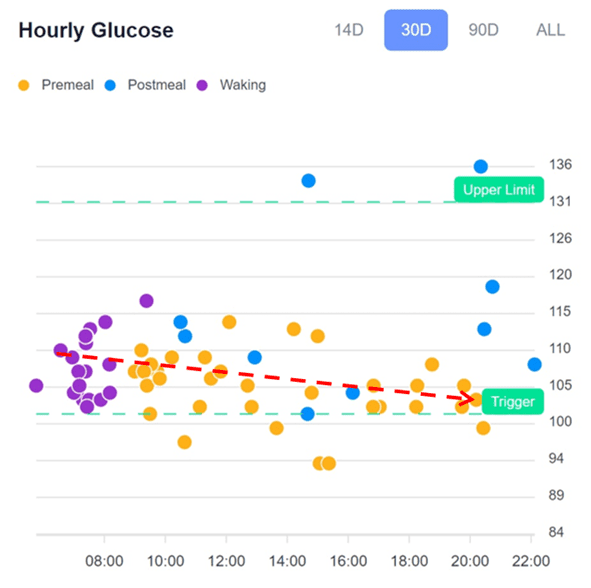
The hourly glucose chart below from the Data-Driven Fasting app shows a typical pattern that we see in the challenges. People will often wake with a higher glucose level in the morning, which is depleted throughout the day. This pattern is particularly common for people on a lower-carb diet with some level of insulin resistance.
Somewhat counterintuitively, reducing fat and allowing some carbohydrates at night often leads to lower waking glucose and less dawn phenomenon the next day.
The hourly glucose chart below, from our Data-Driven Fasting app, shows a fairly typical pattern that we see in people following a lower carb or keto diet in our challenges, with premeal glucose declining across the day. For these people, prioritising protein (which comes with some fat) at their first meal and reducing fat at their last meal tends to help lower waking glucose and reduce the dawn phenomenon.
For more details on why protein may lower blood sugar and our blood sugar and insulin responses to various foods, check out:
- Why Does My Blood Glucose Fall (or rise) When I Eat Protein? and
- Making Sense of the Food Insulin Index.
Aside from prioritising protein, you may also consider not eating so close to bedtime. If you are snacking into the night or consuming a big meal right before bed, you might see higher blood sugars in the morning as your body metabolises the food. This might also interfere with your sleep.
Ultimately, to address insulin resistance and the dawn phenomenon, you need to find a way to lose a significant amount of body fat so insulin can more effectively do its job. In our Data-Driven Fasting Challenges, we guide people to use their glucose before they eat to guide what and when they eat.
In our four-week Data-Driven Fasting (DDF) challenges, we guide people to use their blood glucose meter as a fuel gauge. Over the first three days, you establish your personalised glucose trigger or the average glucose, where you typically feel hungry enough to eat. Throughout the remainder of the challenge, the goal is to wait to eat until your glucose falls just below this value.
If you have a glucose meter, we’d love you to click the link below to try the DDF app and find your trigger today.
Over time, this allows them to use up some of the extra energy they’ve stored on board as high blood glucose, ketones, triglycerides, and cholesterol, so someone can start using some of their body fat for fuel.
Interestingly, waking glucose can sometimes rise in the first few weeks of Data-Driven Fasting as insulin levels drop and the stored energy is released. But over the coming weeks of chasing a lower premeal glucose trigger, weight loss, lower waking glucose, and a reduced dawn phenomenon tend to follow.
As you draw down on all that excess energy, you will see your waking blood glucose come down. As a result, your insulin sensitivity will likely improve, and you may see a smaller long-term rise due to the dawn phenomenon.
Summary
- Dawn Phenomenon is the normal morning glucose rise that ensures your body is fuelled and ready to start the day.
- Insulin-resistant people will tend to see more of a rise in their glucose levels two or three hours after waking.
- You can lower your waking glucose and reduce the dawn phenomenon by adjusting medications and stopping eating earlier.
- Fundamentally, the dawn phenomenon is a symptom of insulin resistance and metabolic syndrome due to excess stored energy.
- You can use your glucose to guide when and what to eat to achieve sustainable weight loss and reduce your dawn phenomenon.
More
- Stress and Cortisol: The Missing Piece to Your Weight Loss and Blood Sugar Puzzle
- Master Your Blood Sugar: A Comprehensive Guide to Managing Carbs for Optimal Health
- Data-Driven Fasting: How to Use Your Blood Glucose as a Fuel Gauge
- Does Coffee Break a Fast? Your Beloved Morning Brew and Fasting
- Personal Fat Threshold Model of Insulin Resistance, Diabetes and Obesity
- What are Normal, Healthy, Non-Diabetic Blood Sugar Levels?
- What Is Insulin Resistance (and How to Reverse It)?




Thank you for such a comprehensive and interesting article. As a T1D I agree that eating late and a fatty meal late in the day makes BSL higher the next morning. But also poor sleep from severe chronic pain or stress, a cup or two of coffee late on the day before and undiagnosed sleep apnoea affect early am to late am BSLs..
What works well for me (if I can avoid the situations above) is a 12 mn dose of Levemir – my cgm, even with some pain through the night can show a very flat line within 3.9 to 6.7 mmol/l. I know that the standard insulin profile of Levemir shows a mild peak about 4 hours after injection and I order whether that helps somehow to detail with the release of cortisol at least in the early am.
Thanks Tony. Glad to see you’ve dialled in your insulin dosing to manage DP. It’s fascinating what we can learn from T1Ds!
Yes, Marty. A real mix of possible factors. I also wonder whether a good night’s sleep gives one a break from daytime stresses. It would interesting to research sleep patterns (levels of sleep – EEGs) to see whether there is any correlation between them and Dawn Phenomenon.
Thank you, Marty. I knew I could rely on you to not only explain it but tell us what to do. I have intermittent fasted for years, skipping breakfast, and initially my blood sugars improved and were in the 80s, Now I’m routinely seeing 103, 109, even though later in the day it’s good. This may not be a huge issue but it worries me. Often I do eat late after dinner because I’m hungry again. I also may be eating too much fat in the evening. I will try to eat some protein maybe mid-morning again and not eat after a more reasonable dinner.
If I routinely go to bed at midnight, what is the latest time I should eat?
finishing eating 2 – 4 hours before going to sleep is a good rule of thumb. you don’t want to go to sleep on a full stomach just after you’ve eaten, but you don’t want to so hungry you can’t sleep.