Get ready to unlock the secrets of blood sugar stability and the magical world of ketogenesis!
Here’s the deal: High blood sugar levels are like the villain in a metabolic thriller, linked to a slew of modern health woes—think diabetes, heart disease, stroke, cancer, and even neurodegenerative conditions like Parkinson’s and Alzheimer’s.
Meanwhile, insulin is the gatekeeper of glucose and ketones in your bloodstream. When you eat, your pancreas cranks up the insulin to store away that excess energy as fat. But when you’re fasting, insulin takes a backseat, allowing your body to tap into its stored energy reserves.
But here’s where things get tricky: When your fat cells reach max capacity and can’t store energy efficiently anymore, you become “insulin resistant.” This leads to energy overflow into places that should remain insulin-sensitive, like your liver, pancreas, heart, brain, and eyes. The result? Elevated glucose, triglycerides, and ketones in your bloodstream.
Enter the concept of ketosis: Exogenous ketosis happens when you load up on dietary fat or supplements to boost your ketone levels. On the flip side, endogenous ketosis is the real star—it kicks in when you consume less energy, causing insulin and blood sugars to drop and your body to start burning its own fat for fuel.
But here’s the punchline: While a low-carb or ketogenic diet works wonders for blood sugar stability, most of the fat-burning magic comes from endogenous ketosis, where you’re torching your own body fat.
So, what’s the secret sauce? Reducing your processed carbohydrate intake is the key to avoiding the clutches of hyperpalatable, nutrient-poor “junk food.” It boosts your sense of fullness, curbs your calorie intake, and makes weight loss a breeze with less struggle.
Here’s the bottom line: There’s no magic number for blood ketone levels, no quick fixes in the form of exogenous ketones, and no need to go overboard with a high-fat “ketogenic diet” if your goal is to burn the fat on your body. The real hero is sustainable, smart eating.
BONUS: FREE Video Lecture “Making sense of the food insulin index”
- Low-carb diets reduce blood sugar levels
- How low should your blood sugars be for optimal ketosis?
- Hyperinsulinemia
- How to manage your insulin load
- Endogenous ketones
- Blood glucose level for optimal ketosis
- Do we get better at using ketones?
- Determining the optimal ketone and blood sugar levels for ketosis
- Blood sugar and ketone blood levels in exogenous ketosis
- How low should your blood glucose be in ketosis?
- Normal blood sugar and ketone range for ketosis
- Virta ketone values
- Optimal blood sugar and ketone levels for ketosis
Low-carb diets reduce blood sugar levels
Many people follow a low carbohydrate diet to manage their blood sugar levels. Foods that contain less carbohydrate cause a smaller rise in blood sugar.[1] [2] [3]
If you have prediabetes or type 2 diabetes, it makes a lot of sense to reduce your intake of carbohydrates to drain the glucose from your bloodstream.
As shown in the chart below from our analysis of the food insulin index data, lowering your intake of carbohydrates tends to lower blood glucose levels after meals.
How low should your blood sugars be for optimal ketosis?
According to mainstream medical definitions:
- “normal” blood sugar is defined as having an HbA1c of less than 6.0%,
- “Prediabetes” occurs when you have an HbA1c between 6.0 and 6.4%, and
- Type 2 diabetes is diagnosed when you have an HbA1c of 6.5% or above.
However, these mainstream definitions of “normal” are far from optimal! Your risk of diabetes, stroke, heart disease, cardiovascular disease and cancer increase with an HbA1c above 5.0%.
By the time you have “prediabetes”, you have an increased risk of many of the most common western diseases of ageing (such as diabetes, heart disease, stroke and cardiovascular disease).[4] [5]
However, simply lowering your blood sugars using medications (e.g. by adding lots of exogenous insulin) does not necessarily reduce your risk.
If you’re interested in pursuing optimal rather than “normal” metabolic health, the table below shows suggested HbA1c and blood sugar targets based on the risk categories for stroke, cardiovascular disease and heart disease shown in the charts above.

Hyperinsulinemia
While elevated blood glucose levels are bad news (due to glucose toxicity and glycation), they also usually go in hand with high insulin levels.[6] [7] [8]
A metabolically healthy person will store excess energy in their fat cells for later use. But in time, after continually consuming more energy than you need, you will get to the point your fat stores cannot continue to expand and absorb more energy from your diet.
Once you exceed your Personal Fat Threshold, you become “insulin resistant”. This means that it takes more and more insulin to store energy in your fat cells.
As you become “insulin resistant” the expansion of your fat cells slows. Your pancreas cannot produce enough insulin to hold the excess energy from your diet in your adipose tissue or stop it from being released into your bloodstream.
Unfortunately, a lower capacity to gain high levels of body fat is not as good as it sounds. Once your fat cells are full, any excess energy will be redirected to other parts of your body that are still insulin sensitive (e.g. your liver, pancreas, heart, brain and other vital organs).
Your pancreas then has to work overtime, secreting more and more insulin to hold back your stored energy while you use up the energy in your bloodstream that continues to be topped up from the food coming in via your mouth.
How to manage your insulin load
The good news is that you can tailor the insulin load of your diet to help you stabilise your blood sugars.
Managing the insulin load of your diet can be particularly useful if you inject insulin to control your blood sugars. It is almost impossible to match large bolus insulin doses with large amounts of dietary carbohydrates and protein.
Trying to match large amounts of carbohydrates with large amounts of insulin leads to large errors, while a smaller intake of carbohydrates requires smaller amounts of bolus insulin and smaller errors, which are easier to correct.

A person with type 1 diabetes cannot produce enough insulin to keep energy locked away in their liver and fat stores. Without exogenous insulin, they will see both their blood sugar and blood ketone levels rise as their stored energy leeches into their bloodstream.
As shown in the image of “JL” below (one of the first children with type 1 diabetes to receive insulin treatment), people with type 1 diabetes quickly regain weight with exogenous insulin.
If you inject insulin, you need to think about finding the optimal dose of insulin required to keep your blood sugars stable.
- Too much insulin can slow the release of fat from your body to be used for fuel; your blood sugars will drop, and you will feel compelled to eat.
- With too little insulin, you will effectively disintegrate, with all your stored energy pouring into your bloodstream.
This insulin-centric view of diabetes management and obesity falls over because it doesn’t translate to someone who is not injecting insulin.
Your pancreas will not secrete more insulin than it needs to hold back your fat in storage while your body uses up the energy coming in from your mouth.
A low-carbohydrate diet helps to stabilise your blood sugars. However, if you want lower blood sugars and insulin to truly reverse your diabetes, you need to find a way of eating that keeps you satiated while still getting the essential nutrients you need to thrive.
Endogenous ketones
When you go without food, the glucose stored in your bloodstream, liver and muscles (glycogen) is depleted to healthy levels.
Then, once the excess glucose is used up, your body will turn to your body fat stores for fuel. Your liver then converts body fat to ketones to use as an alternative fuel to glucose for use by the brain, heart and other vital organs.
This process is known as “endogenous ketosis” (note: endogenous means that the ketones originate from inside your body).
Most of the beneficial effects of a ketogenic diet occur during endogenous ketosis (i.e. autophagy, mitogenesis, mitophagy, upregulation of SIRT1 and increase of NAD+). Your body goes into repair mode to ensure it can survive to procreate when food is more available.
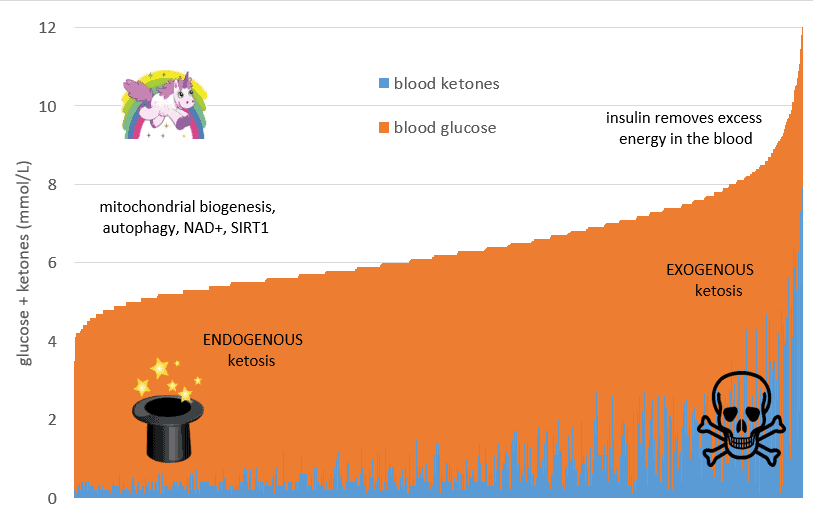
The chart below shows my blood sugar and blood ketone levels (BHB) during a seven-day fast. As glucose levels decrease, blood ketone levels are produced to compensate for the lack of energy from your diet. The sum of glucose and ketones can be thought of as the “total energy” (i.e. glucose + ketones = total energy).
When fasting, your body may allow the total energy in your bloodstream to go to drift up quite a lot. This enables you to be ready at a moment’s notice to hunt or gather food to survive. However, we can not mimic energy restriction’s benefits by adding extra fat or exogenous ketone supplements.
Your pancreas will raise insulin to manage your blood sugars and ketone levels and keep your body fat in storage while you use the energy from the food from your diet, regardless of the source.
Blood glucose level for optimal ketosis
Our understanding of the ketogenic diet is evolving quickly as “keto” has grown in popularity. However, there is still a lot of confusion around what constitutes optimal ketone levels.
While many people are eager to try a ketogenic diet, the reality is that it is hard for most people to achieve and maintain what are commonly considered to be “optimal ketone levels” (i.e. 1.5 to 3.0mmol/L according to this ketosis chart from The Art and Science of Low Carbohydrate Performance) without extended fasting or continuing to add more and more refined dietary fat.
But the problem is that prioritising more dietary fat is typically counterproductive over the long term if your goal is weight loss or diabetes management. Before long, you’ll likely find that you are putting on extra body fat, which in turn will lead to higher insulin levels and elevated blood sugar levels.
I had the privilege of having Dr Steve Phinney (pictured below in our kitchen making his famous blue cheese dressing) stay at our place recently for a couple of days when he spoke at a Low Carb Down Under event in Brisbane. During this time, I quizzed him about the background of his optimal ketosis chart.
Steve said the optimal ketosis chart (shown above) was based on the blood ketone levels of participants in two studies done in the 1980s. One was with cyclists who had adapted to ketosis over six weeks and another ketogenic weight loss study. In both cases, these ‘optimal ketone levels’ (i.e. between 1.5 to 3.0 mmol/L) were observed in people who had recently transitioned into a state of nutritional ketosis.
However, as more people try a low carb or ketogenic diet, many people find that their blood ketone levels continue to decrease after a few weeks or months.
necessarily lead to weight loss and that there is limited use in tracking them!
Do we get better at using ketones?
Urine ketone strips (which measure acetoacetate in the urine) are considered by many to be of limited use because before too long, the body stops excreting ketones into the urine as it learns to use them rather than wasting them.

It seems that your body also adapts to use blood ketones more efficiently the longer you follow a lower carbohydrate diet. Most people move beyond the ‘keto adaption’ phase as their bodies learn to use fat more efficiently, and their ketone levels reduce further.
You can think of BHB as the storage and transport form of ketones. Your body converts BHB back to acetoacetate to be used for energy.
The BHB ketones you measure simply tell you how much energy you have stored as ketones in your bloodstream. Unfortunately, it doesn’t tell you anything useful about your ability to burn fat for fuel. High blood ketones may mean you have unused fuel backing up in your bloodstream (which is usually not a good thing).
Just like a fuel-efficient car doesn’t need a massive fuel tank, you don’t need high levels of ketones or glucose in your bloodstream if you have a healthy and efficient metabolism.
Determining the optimal ketone and blood sugar levels for ketosis
Back in 2014, I was eager to experiment, learn and do whatever I could to lose weight and optimise my health.
But I was still confused after reading everything I could. I had become much fatter after pursuing ‘optimal’ ketone levels’ (see my work profile pics below), so I decided to compile some data from my own testing and online friends who were also tracking their blood sugar and ketone levels.

I wanted to understand what typical ketone blood levels were for people who had been following a reduced carbohydrate diet for a while. After I shared this initial data, other people sent me their data to add to the chart. Then, Michel Lundell from Ketonix shared an extensive set of anonymised data from people following a ketogenic diet.
The chart below shows the sum of the blood sugar and ketones (i.e. total energy) from nearly three thousand data points from a broad range of people following a low carb or ketogenic diet. Blood ketones are shown in blue (on the bottom), while glucose is shown in orange (on the top).
On the right-hand side of the chart, we have a high-energy state where both glucose and ketones are elevated. This high-energy situation is similar to someone with Type 1 diabetes with high glucose and ketone levels due to inadequate insulin.
Note: Diabetic ketoacidosis is diagnosed when we have glucose levels above 15 mmol/L or 270 mg/dL and ketones above 0.5 mmol/L. This would equate to a total energy in the bloodstream of 15.5 mmol/L.
On the left-hand side of the chart, we have people a lower total energy state. It seems that because they store and burn fuel efficiently, these metabolically healthy people don’t need large amounts of fuel circulating in their bloodstream.
Based on the analysis of this crowd-sourced data, it seems the average blood sugar value for someone on a low-carb diet is around 4.9 mmol/L (or 88 mmol/L) with a ketone blood level (BHB) of about 1.5 mmol/L.
Blood sugar and ketone blood levels in exogenous ketosis
Some people come to low-carb or keto for therapeutic purposes (i.e. to manage chronic conditions such as cancer, epilepsy, traumatic brain injury or dementia). These people may benefit from higher ketone blood levels to fuel the brain when glucose cannot be used efficiently.
If you are trying to avoid muscle wastage that occurs in cancer cachexia or trying to feed a growing child who has epilepsy, an energy-dense high fat low satiety diet can be an advantage to gain weight (after cancer treatment) or grow (in the case of a child who has epilepsy). However, most people do not require therapeutic ketosis, particularly if weight loss, improved satiety or blood sugar control is the highest priority.
People following a therapeutic ketogenic diet may choose to load up with MCT oils and other added fats to achieve high ketone levels and low glucose:ketone index values (GKI) values. Others target high levels of ketones for brain performance or load up on exogenous ketones and glucose together to ‘dual fuel’ for elite athletic performance.
This over-fuelled state with elevated glucose and ketones is shown in the chart below from the people with the highest total energy.
While it may be useful if you’re about to race in the Tour de France, chronically elevated energy from glucose and ketones is not ideal, particularly if you are sedentary, trying to lose weight or reverse your type 2 diabetes.
One of the benefits of a low-carb diet is that it largely eliminates hyper-palatable processed foods that are typically a combination of refined starches and vegetable oils. As shown in the chart below from our satiety analysis, the most hyper-palatable foods are generally a combination of refined carbs and fat.
The danger, however, with trying to drive high levels of ketones by eating more fat is that it will lead to an energy excess intake which will drive up insulin and promote fat storage. Foods that contain a higher percentage of fat do not typically lead to greater satiety.

Reducing your carbohydrate intake can help you to avoid carb+fat hyperpalatable junk food, increase satiety, help you to eat less and lose weight. However, pushing carbohydrates to very low levels can lead to lower satiety and increased energy intake.
So, while reducing carbohydrates is beneficial if it moves you away from hyperpalatable processed foods that are a combination of carb+fat, too much dietary fat will not be optimal if it leads you to significantly increased energy intake.
How low should your blood glucose be in ketosis?
Many people embark on a ketogenic diet in the hope of managing their diabetes and losing weight. They want lower insulin levels to enable them to burn more body fat for long-term insulin sensitivity and health.
On the left-hand side of the total energy chart below, we have endogenous ketosis (meaning that your body fat is being burned for fuel). With lower levels of energy in your blood, your body will draw on your fat stores to make up the difference, as well as using excess stored fat and old proteins in your liver, pancreas, brain and other organs (i.e. autophagy). This is a great place to be if you are trying to reduce your blood sugar or lose body fat.
Normal blood sugar and ketone range for ketosis
After analyzing thousands of ketone measurements, we bring you the Ketone Levels Chart!. The data is divided into five quintiles, from the lowest to the highest total energy.
For each quintile, I have calculated the average, 25th percentile and 75th percentile blood ketone (BHB) value (i.e. half the values fit between the 25th and 75th percentile).

If you are on a ketogenic diet and relatively metabolically healthy, you may see BHB ketone values between 0.3 and 1.5 mmol/L. Ketones will be higher if you are fasting, restricting calories, exercising or consuming more dietary fat than usual.
However, remember that blood ketones will probably decrease over time as your body adapts to burning fat and ketones more efficiently. So, try to resist the temptation to add more extra dietary fat to maintain elevated ketone levels.
Virta ketone values
It’s interesting to note that the crowd-sourced data above aligns well with ketone data from the Virta study one-year results (Phinney et al., 2017), where they aimed to get participants with diabetes into nutritional ketosis to improve blood sugar management and reverse diabetes.
The distribution of BHB levels over the first ten weeks of the Virta trial is shown in the chart below. While there were some higher ketone values, many people also had values of less than 0.5 mmol/L.
In spite of consuming a “ketogenic diet” under the supervision of the Virta team, most of the study participants did not achieve ketone levels that qualified as “nutritional ketosis” (I.e. BHB > 0.5 mmol/L).
The chart below shows the average Virta results over the first year, with ketones rising from 0.18 mmol/L to 0.6 mmol/L initially but then decreasing to less than 0.3 mmol/L after a year.
The Virta study two-year results show that blood ketone levels remained at 0.27 mmol/L after two years of a ketogenic diet. The chart below summarises the change in ketone values over the two-year duration of the study.
While the participants in the Virta program initially saw an increase of blood ketones into the ‘nutritional ketosis zone’ (i.e. greater than 0.5 mmol/L) on average after ten weeks, their blood ketones settled back to just above the control group on the standard western diet. At no time did their ketone values approach the optimal ketone zone (i.e. 1.5 mmol/L according to the commonly accepted definition of ketosis).
We have also seen a similar trend in our Nutrient Optimiser Challenge, with blood ketones rising initially over the first couple of weeks of weight loss when people focused on high-satiety nutrient-dense meals. But after a few four weeks, blood ketone levels decreased as people continued to lose weight and lower their blood sugars. It seems that once your body uses up the excess energy (both glucose and ketones) in your bloodstream, it can get on with using body fat.
It was interesting to see that the people who identified as insulin resistant tended to have slightly higher blood ketone values than those who said they were insulin sensitive.
It seems that people who are physically fit and metabolically healthy may tend to have lower blood ketone levels as well as lower blood sugar levels, especially after they have been following a low-carb or ketogenic diet for a while.
However, regardless of blood ketone values or whether people believed they are insulin resistant, the data from the Nutrient Optimiser Challenge also showed that people tend to lose weight at a similar rate regardless of whether they identified as insulin resistant or insulin sensitive.
Optimal blood sugar and ketone levels for ketosis
Unless you are managing a chronic condition that may benefit from elevated ketone levels (e.g. Alzheimer’s, Parkinson’s, dementia or epilepsy), you could potentially save a lot of money and angst by focusing on keeping your blood sugars closer to optimal and not worrying about your blood ketone levels.
In line with oxidative priority, the glucose in your blood needs to be burned before the fat in your diet and the fat in your body. If your glucose stores are constantly overfull, you will be ‘stuck’ burning glucose, and you will not get to use your body fat.
Once your blood glucose has stabilised with a reduced carbohydrate diet, you can then prioritise high satiety, nutrient-dense foods and meals to continue to lose weight and reverse your diabetes.

Any thoughts on physiological insulin resistance for those doing ketogenic diets over the long term?
I have been doing a ketgenic diet (565 days+) with all days having a blood ketone fasting level over 0.5 or greater with the average around 1.8. Over time the levels are reducing while fasting glucose is rising. I still test my fasting blood ketone as over 0.5 but it tends to range in the 0.8 to 1.3 range. I am careful with my tracking so my macros are always 80%+ fat with low protein and carbs.
Just curious to anyone’s thoughts on this……
Thanks
Stats: Female/36 yrs/5’8/117 lbs
Not an issue.
A good summary of it here:
https://twitter.com/CarnivoresCreed/status/622184077223833600
Some more thoughts on the issue of physiological insulin resistance here – https://optimisingnutrition.wordpress.com/2015/06/08/physiological-insulin-resistance-and-coffee-addiction/
There are a number of possible issue here.
This paper from Seyfried indicates that a ketogenic diet with excess calories can be an issue. If this was the issue then fasting or cutting back on total calories could be a consideration. It would be interesting to know if you were gaining weight as well as having rising blood sugars. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1819381/
What about insulin levels? C-peptide? Is the pancreas burning out.
I have also heard Peter Attia discuss this sort of thing but there isn’t much other detail about why a long term keto diet might not trigger insulin resistance.
“Excess calories”, but consider the source: KetoCal
http://www.myketocal.com/ketocal4-1.aspx
Whilst they can be interesting, I really don’t like conclusions based on junk keto meal replacement stuff primarily based on processed ingredients and seed oils.
Noted Ash. Do you have any thoughts on why blood sugars might be drifting up while fat is at 80%. Personally I wonder if it might be better for long term health to run at higher levels of protein (with the proviso that your pancreas can keep up) to maximise nutrients.
Actually I have continued to lose weight my bmi is currently 17.6 so no weight gain and I eat at a caloric deficit, I weigh my food and track it carefully which is why I was curious about this specific phenomenon so that I look at any high correlations with changes in my glucose and ketone blood levels
Kathy, do you know if you get higher blood glucose levels with higher protein levels while keeping carbs low? There is heaps of useful nutrients in protein foods that would be good to maximise while keeping within the capacity of your pancreas to keep up. Have you don’t any matched ketone / glucose testing to know what your GKI number is? I would even be interested in adding your data points to this chart?
I stay on the super low end of the protein spectrum usually lower ranges for the therapeutic benefits of ketosis 30-45 g per day (under the 0.5 x lb/lean body mass).
I have only increased my cals from fat when I went to under weight. Main sources of fat being mct oil, ghee, coconut oil, olive oil, avocado & avocado based products. I have started to consider keto supplements like ketocana but on the fence still.
Have you tried intermittent fasting to reset insulin sensitivity? Seems your insulin load is pretty low though so that’s unlikely to be a problem.
I think it’s probably ideal for most to be at a higher protein intake to increase nutrients, though if you need the therapeutic benefits of keto that’s a whole different issue.
I think the KeotoForce KetoCaNa is fascinating technology! I got the KetoCaNa in the mail the other day. I have tried it twice. Just a little seemed to kill my appetite for the day! My type 1 diabetic wife tried it and it gave her gut upsets (autoimmune – more sensitive). I’m looking forward to experimenting with it in the future.
Can’t seem to reply to your reply directly, dunno where this will end up in the stream…
In the “keto science” communities we’ve come to a gentleman’s agreement to refer to it as adaptive glucose sparing as the term insulin resistance is too scary – much like many medicos and nutritionists are still freaked out by the term ketosis by conflating it with ketoacidosis.
Eventually it’ll be more widely accepted the nature of insulin:glucagon ratios and such, and why protein can be insulinogenic and even raise blood sugar somewhat, but it’s not really an issue in sane amounts.
I’m guessing you’ve been following the Unger stuff already.
Have seen a video by Unger on type 1. Interesting stuff.
My main interest with protein being insulinogenic is for type 1 diabetics calculating their doses, but I think it’s relevant to some degree for type 2s who might benefit from moderate rather than high levels of protein to manage blood glucose levels.
Is there any further keto science out there on blood glucose levels drifting up after a long period on strict keto? Jimmy Moore is another interesting case in point. I don’t think it’s a big deal if everything else is going along fine. It would seem to just be a way that your body decides to run at higher blood glucose levels?
Yeah I’ve been asking for more N=1’s from T1s with regard to protein intake for a while. From a purely observational standpoint it seems like mostly a non-issue. In T2s I don’t see how it could be an issue, if you’ve already got your carbs down to ketogenic levels the amount of protein you consume is never going to have any real effect on BG/insulin – relatively speaking. Some might benefit from an intervention period of a week or month of 4:1 keto, but for the most part cutting the carbs is going to do 90% of the work.
There’s a fair bit of stuff out there regarding “physiological insulin resistance” and BG float. Again it’s something we’ve come to redefine as benign in the absence of exogenous carbohydrates at worst, and likely a beneficial trade-off in the long-term.
As for Jimmy – I respect what the guy has done for the community overall, but I’m over the fascination and don’t really consider him an N=1 to follow. 3 years ago I wrote of my misgivings about him probably about to become “our” new ambassador: https://www.reddit.com/r/keto/comments/v2owk/after_8_years_as_a_lc_guru_jimmy_moore_finally/c50rxk1
I suppose my interest in the GNG issue was sparked by seeing a lot of type 1 diabetics struggling to manage their blood sugar response to protein.
See this draft article for more on that – https://www.dropbox.com/s/1cl533l2dzb1dzy/Advanced%20dosing%20for%20type%201s.docx?dl=0
Agree that the nutritional value from protein is highly desirable, but in the absence of exogenous medicating it seems to be a balancing act between maximising nutrition and overloading the system.
Type 2s certainly seem to struggle to deal with protein more than healthy people. See https://optimisingnutrition.wordpress.com/2015/06/15/the-blood-glucose-glucagon-and-insulin-response-to-protein/
It’s interesting to note that Metformin works by limiting GNG! http://www.nature.com/nature/journal/v510/n7506/full/nature13270.html
http://www.marksdailyapple.com/does-eating-low-carb-cause-insulin-resistance/#axzz3gYUnhmZn
There’s not a lot written on PIR, however it usually refers to what happens when someone who is eating low carb then goes and has a significant amount of carbs and their blood glucose levels shoot up.
This is not the case for Kathy as she is just continuing with her therapeutic keto diet.
The issue could be pancreatic burn out which the c-peptide test would confirm.
I also wonder if someone at extremely low protein (i.e. very low glucose) is not getting the nutrition they need and this can lead to other issues.
I plan on increasing protein a bit and tweaking a few other items (IF I have experimented with but didn’t find an impact on trend line; tried the true fast and tried the modified version with bulletproof coffee).
I feel great health wise no issues with energy, mental clarity, sleep etc. (with some data & tracking ocd still lurking lol)
Another interesting correlation I will throw out there to see if anyone else is quirky. When I travel for work (flying only car rides do not do this) my ketone levels sky rocket even as I increase water greatly I assume it has something to do with dehydration.
I’ve just got a glucose meter. And I am still working my way through manual. Lol. But I think I should have got one that tests for ketones too. Although I read somewhere that you can get a good idea just from blood glucose. Oh and I’ve got pee strips. Which are showing deep purple. Do you think I can just track blood glucose or should I shell out for the ketone meter to get my ketone /glucose index
Can’t wait till someone just makes an iPhone app to do this.
Ketones are interesting but I think is probably ideal to focus on get get your blood sugar down initially. The chart in this article will give you an idea of what your ketones might be.
I think this a really useful development of your thoughts. I will certainly be using the GKI ratio myself, to see how I go. My recently started ketone tests seem to vary quite a bit: I don’t know if that is a common exoerience,
I am a 62 yr old T2 DB in the UK, who is managing my diabetes with LCHF, fasting and HIIT exercise. I am a retired engineer (so I can make time available), and feel much more comfortable to work with some numbers that mean something to me. I have only recently started measuring ketones: the “ketone” label scared me off, until I educated myself. Last HbA1C was 5.1% (32) and my general wellbeing is transformed. As time goes on, I am looking much more at the wider health benefits of LCHF and a ketosis diet, and not just T2DB management.
As a T2DB, I have often wondered what is the balance of my diabetes, between insulin resistance and low insulin production.
One of the problems in the UK is that the tests available are fewer than in the USA. It is very difficult to get even one fasting insulin test, so something that is proximal is very useful.
Thanks Dave. Let us know how you go. I’m eager to add to this dataset as I think understanding the relationship between ketones and glucose is useful, even if just to save money on ketone testing.
GREAT blog.
What time of day are the ketone & glucose levels tested? Are these fasting (am) levels?
I am in very similar situation as Kathy above.
Correct, I take my levels completely fasted in the morning so that mct oil and other ingested fats are not contributing to the blood ketone levels.
My fasted state is usually 12 hours + with my last meal around 6 or 7 at night.
I was usually testing in the morning before food, but sometimes during the day too. I agree that it’s probably better to test in the morning for consistency without the food having an impact. Although I found typically my ketones increased through the day.
Thank you for the time you spend in putting together this information. Unrelated but the mention of Rosedale reminded of a question re exercise. Rosedale says you should exercise after meals to burn the excess, Keifer says resistance exercise before exercise is optimum for T2. Before or after, what do you think?
Oops sorry that should be Keifer exercise before eating..
Rosedale and Kiefer are pitching at two very different audiences. Depends if you are sick/diabetic/obese or bodybuilder/figure competitor. A lot of Kiefer’s stuff is about getting an insulin surge to build muscle after periods of extremely low insulin. Most people just need to drop some weight and reduce their overall insulin load.
I used to dismiss Kiefer as irrelevant to me ie for bodybuilding bros however if I look beyond that he is quite interesting, a lot of his research has been based on diabetic papers. Here https://www.youtube.com/watch?v=dXDEPc38y08 at point 33.50 mins he talks about resistance exercise before meals as being “life changing for T2s”.
I think the priority for type 2s would be to do some training. So whenever it works for you and feels good is probably the priority.
Resistance training will burn through glycogen stores which are going to be full for most type 2s regardless of whether it’s before or after.
For bodybuilders he’s saying to work out fasted and then eat afterwards to stop the ongoing breakdown of the muscles. Not as much of a priority if you’re not walking around most of the day with depleted glycogen.
If fasting insulin levels are low (say 3uIU/mL), how can you be certain it may not be bcs your pancreas is unable to secrete enough insulin to keep glucose levels in check (like with Kathy’s gradually increasing FBG numbers)? Is the only way to know is with C-Peptide test and/or GAD65?
Would they be definitive?
Yeah. I’m not a doctor, but a c-peptide test seems logical to confirm that the pancreas is still functioning. If Kathy is using keto for therapeutic purposes (autoimmunity) it is possible that the same issue is also degrading her pancreas.
Hi Marty,
I got a question about your chart on Average glucose and ketones. Is that for fasting BS? Or average a day?
Thanks 😉
Mónica
Average across the day. When I was testing my blood sugar levels I’d just average all of them to estimate HbA1c.
Hi I’ve just recently been on the ketogenic diet for about 6 months working with Dr. Fung because I have type 2 diabetes and not sure if I’m Keto adapted or not yet. This morning I tested my ketones and they were a 2.7 mmol and my blood glucose was a 6.0 mmol. Any thoughts as to why this is since I thought if ketones went up blood glucose should go down? Could it be that my body is still not Keto adapted?
Thanks,
Eric
I assume you’re doing fasting if you’re with Dr Fung. Sounds like you’re off to a great start. It will just take time to burn through your stored glucose and fat.
This video from Bob Briggs is helpful to show you how you will progressively burn through your glucose and improve your insulin resistance. https://www.youtube.com/watch?v=SDzJKaBvOGw
Lots of people benefit from keto initially. Eventually you will want to see if you can build up your protein levels slowly to a point that you can heal your body and improve your insulin resistance with good food as well as fasting.
Well look and you shall find. My fg was 90 ies with less than .5 ketone. A1c 5.7, so today i did glucose and ketone 2.5 hr after my lg meal. Glucose 84 (4.6) and ketone .7. With a GKI of about 6.6. Does this sound right, maybe im missing something, but I’m pretty sure im keto adapted. I need positive feedback, my A1c has got me bummed. Also, fg seens to be higher than evening glucose.
Sounds all good. Some fasting or an overall reduction in calories may help to bring down the glucose and up the ketones more.
Hi Marty.
Keep up the good work I find your stuff very useful.
My 2 cents on Glucose/Ketones.
I have been restricting carbs for about 2 years now but have found it difficult to get ketones much above .5 mmol/l, even with glucose around 5 mmol/l. This was eating 1 or two meals a day and snacks.
This changed dramatically when I went to 1 meal/day and fasting for 2 days/week. Ketones went to and stayed between 2-5 and glucose dropped further to about 4.6.
Seems like a harsh regime but it actually isn’t. I never feel hungry weight is stable, I look forward to the fasting days as energy goes up and my mood elevates.
We will see.
Thanks for all your info.
Tim.
That’s great. Sounds like you’ve found the ideal regime for you. Many people will need to incorporate fasting as well as a low carb / low insulin approach.
im still learning about diet and fast relate to ketosis, can i know it is normal if glucose level 3.3 after 3 days of fasting. im just consuming water only in 3 days. it is extra supplement (magnesium and potassium) needed during my fasting ? i planning to do 21 days of fasting ( just consume water only)
Very interesting piece. I was directed here after increasong ketone levels. I eat a Low Carb High Fat diet, and do not fast as such. Some days I may naturally do intermittent fasting, just due to lack of hunger. My blood glucose levels have consistently been in the 3s, and my ketones are usually in the mid 2s at their lowest, but over the last few days have been in the 4s and even as high as 5.2.
I am a bit concerned as my fasting is 76 and would not rise above 78 even after I eating and would remain between 76 and 78 all day unless I dont eat or if I eat a low fat meal. I have tried researching but I have not come accross a definitive answer as to why fasting/not eating would raise my blood sugar. I have been on the ketogenic diet for 2 months now and would like some advice.
Thanks,
Regards
Vivian Peters
That blood glucose is on the low side of average but if you feel fine may be nothing to really worry about.
FBG – 85
A1C – 5.5%
Is there a disconnect between the two numbers?
Yeah, based on that one FBG value you’d expect your HbA1c to be about 4.7%, however HbA1c is based on your sugar values over the past three months. There isn’t always a direct relationship though as there are other factors that influence HbA1c.
http://www.diabetes.co.uk/hba1c-to-blood-sugar-level-converter.html
https://chriskresser.com/why-hemoglobin-a1c-is-not-a-reliable-marker/
Hello Marty,
I’ve been doing Keto since Sept. In the past month I have started IF – usually 24/1 eat lunch only with a tea for breakfast with a tb of coconut oil or MTC. I have no medical issues other than overweight. My BG is always around 3.4- 3.6 and ketones get as high as 7.1
Is this ok?? I’ve asked this question on so many fb pages and no one seems to be able to answer me – I am hoping you will.
Thank you so very much!!
Sheila
Do you feel and look OK? That level of ketones would be of more of a concern if your BGs were high too. Seems your insulin levels are very low. If your insulin levels are too low then you may be losing muscle mass and too much weight. If this was as problem you could see how you feel with a bit more protein and green vegies.
I’ve been doing low carb for about 4 months now and I have lost over 70lbs. I’m pretty sure that I am/was insulin resistant. I have done two fast so far, one lasting 7 days and the other 4 days. I usually IF daily if I’m not doing a water fast. My question is, I saw a video by Dr. Jockers that stated that you’re not in NK with a bg of 80 and above. My fbg is usually 79-84 again unless I’m on the water fast. My bg is usually 65. Is a bg of 83-87 optimal for nk? What would the ketone be? I dont have a ketone meter.
The table above shows the relationship between Ketones and glucose. Sounds like you’re in a pretty great place. If you try to chase higher ketones with more dietary fat you may stall your fat loss. Glucose may come down a little but more with more fasting and weight loss.
Are you still wanting GKI numbers? I’ve been tracking the past 3 weeks and will continue for a while yet. Average seems about 5 which seems great but I’m T2D with NAFLD so must be IR?? Expected a higher number.
That would be great. Would love some more data. Looking at a few more articles that will use that data. Send to martykendall@outlook.com
Hi
Please can people comment on the best time to test. I understand the best time in the morning fasted but not sure I understand why. Wouldn’t it be better to test after eating? And if so at what point?
Thanks charlene
You are going to get a lower GKI after a period of fasting. The GKI is really a proxy for fasting insulin levels.
Marty I am a type 1 diabetic (25+years) and recently started measuring my ppm acetone every morning (ketostix). How do I use this information and what is it tell me about my LCHF diet?
Keeping minimal ketones in the urine mean you have adequate insulin on board so as not to be going into ketoacidosis. It’s more your blood sugars that will help guide your food choices.
Great post! Quick question…
I was always under the impression that eating globs of fat would only prevent the body from burning it’s own fat but that it still wouldn’t affect insulin whatsoever.
Are you saying that the production of ketones is not demand-driven but more so supply-driven, and that more fat consumed = more ketones in the blood = higher insulin response?
Also, in regards to PSMF, would 0.8g/kg prevent LBM loss in the absence of carbs/fats, or is it necessary to raise protein?
I’d like to know the answer to these questions too..
Beuler..Beuler..?
I am a female competitive athlete, (WBFF cat. Bikini) – last season I followed a typical prep with a coach defining my macros. High protein / mod. Carbs / low fat.
I was happy with my results and placed 4th in my category. For the past months I have been on a keto protocol to rehabilitate my messed up metabolism thanks to the ridged dieting of a bodybuilding athlete.
So far I am almost 3 months into a keto protocol and I love it.
I’m still adapting, so lifting heavy is quite the challenge.. but I know that with improve once my brain has made the switch to burning ketones.
Otherwise all the benefits of a keto protocol are enough to never want to go back to being a glucose burner.
The lack of mental clarity, sugar cravings and inflammation was anightmare. I am thankfully free from all that. No more cravings, no more dependence on thermogenics or caffeine. I don’t even sip on BCAAS anymore.
My keto macros are 80f/15p/5c – carbs coming from cruciferous vegs.
I measure blood glucose and BHB with a monitor.
My questions:
1. I am having hard time finding legit information for FEMALE weightlifters and how to calculate adequate protein. (I’m tall )
2. Is it possible to put on muscle mass on a keto protocol? (without “carb loading” – or taking glucose before a workout)
I’m not aware of any differences for females. You will crave more protein if you are lifting. Have a look at this article. If you focus on nutrient dense foods you will get more than enough protein. You may struggle to build muscle if your definition of keto is heavy on the refined fat. https://optimisingnutrition.com/2017/06/09/how-much-protein-is-too-much/
My Hba1c went up on keto and physiologic IR is through the roof. Im eating no enriched carbs. My training and work is at play. Im confounded. Nearly 36 months LC, and 2 years SKD. Vision is blurry too. Told I was undereating? Yet IM slowly getting bigger. I gained 6lb muscle 5 lbs of fat trying CKD stuff (via DXA). Now Im strict. That said I feel really good. My body comp? Look like out of a movie. So I mention stuff isnt right but whats up? Finally got my nutrition almost 100% right. Soon Ill throw the data in the ON algorithm see where I add up… Love your site Marty. Legend
There is too much scatter in the glucose and insulin charts to be useful. From the glucose chart I would be better off eating an orange than an egg and in the insulin chart I could eat raisins or steak. In both there does not appear to be clear correlations.
Marty, thanks for the excellent article. Though I’m bit puzzled about your statement: ” But keep in mind that most of the good things we attribute to ketosis and the ketogenic diet occurs due to endogenous ketosis when fat is coming from our body. ” OK, So if we are already healthy at our ideal body weight and ideal body fat, then ketogenic diet does not offer as much benefits since then we will not be restricting calories and all fat will be coming from outside? thanks
My Keyone is 4.1 should I be worried
How are your blood sugars? Are you gaining or losing weight?