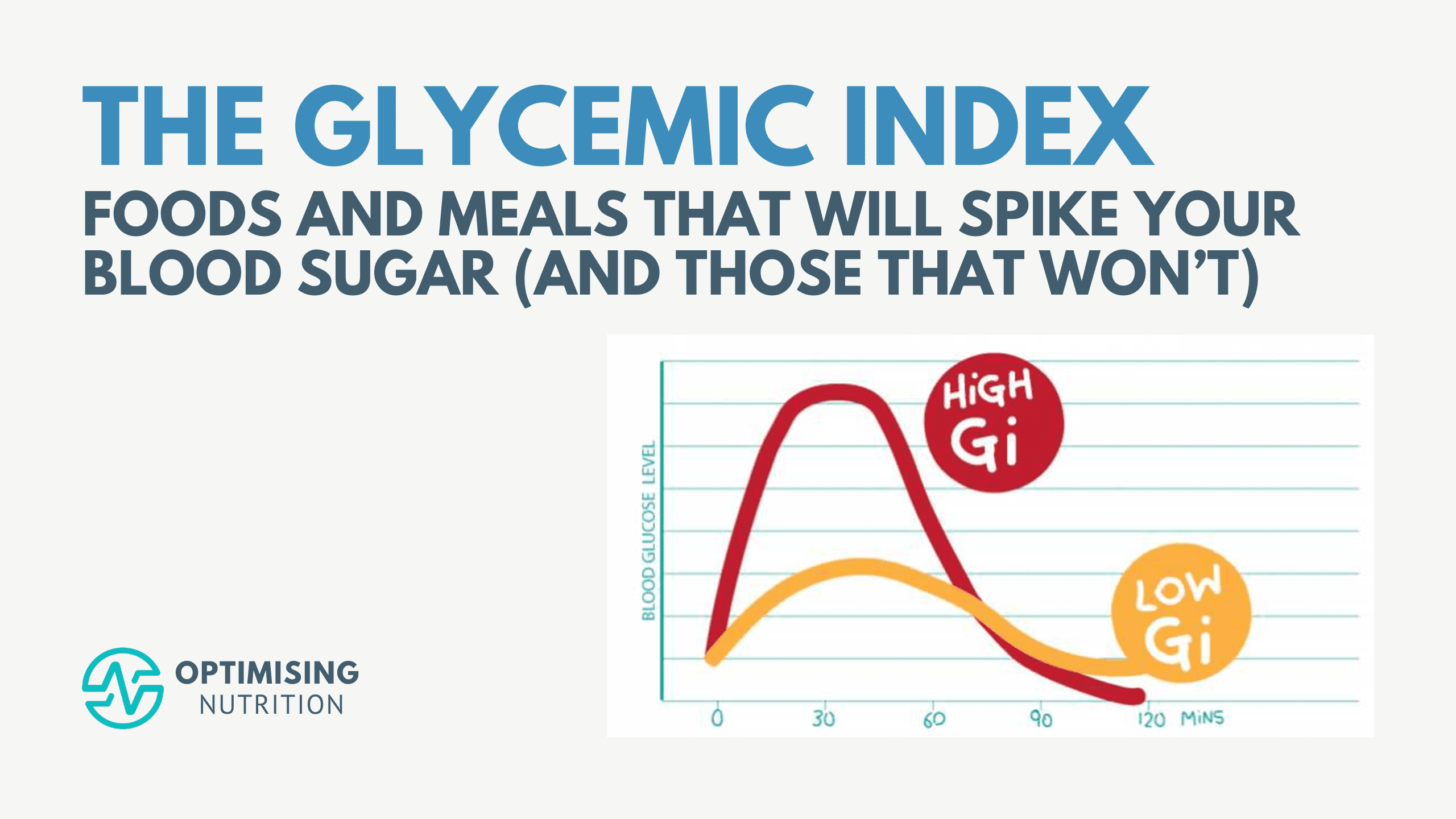
Beyond the Glycemic Index: Exploring the Glucose Score
Discover the Glucose Score, an innovative tool transcending the traditional Glycemic Index to help manage blood sugar levels effectively. Learn how to leverage both metrics for better blood sugar stability post-meal.