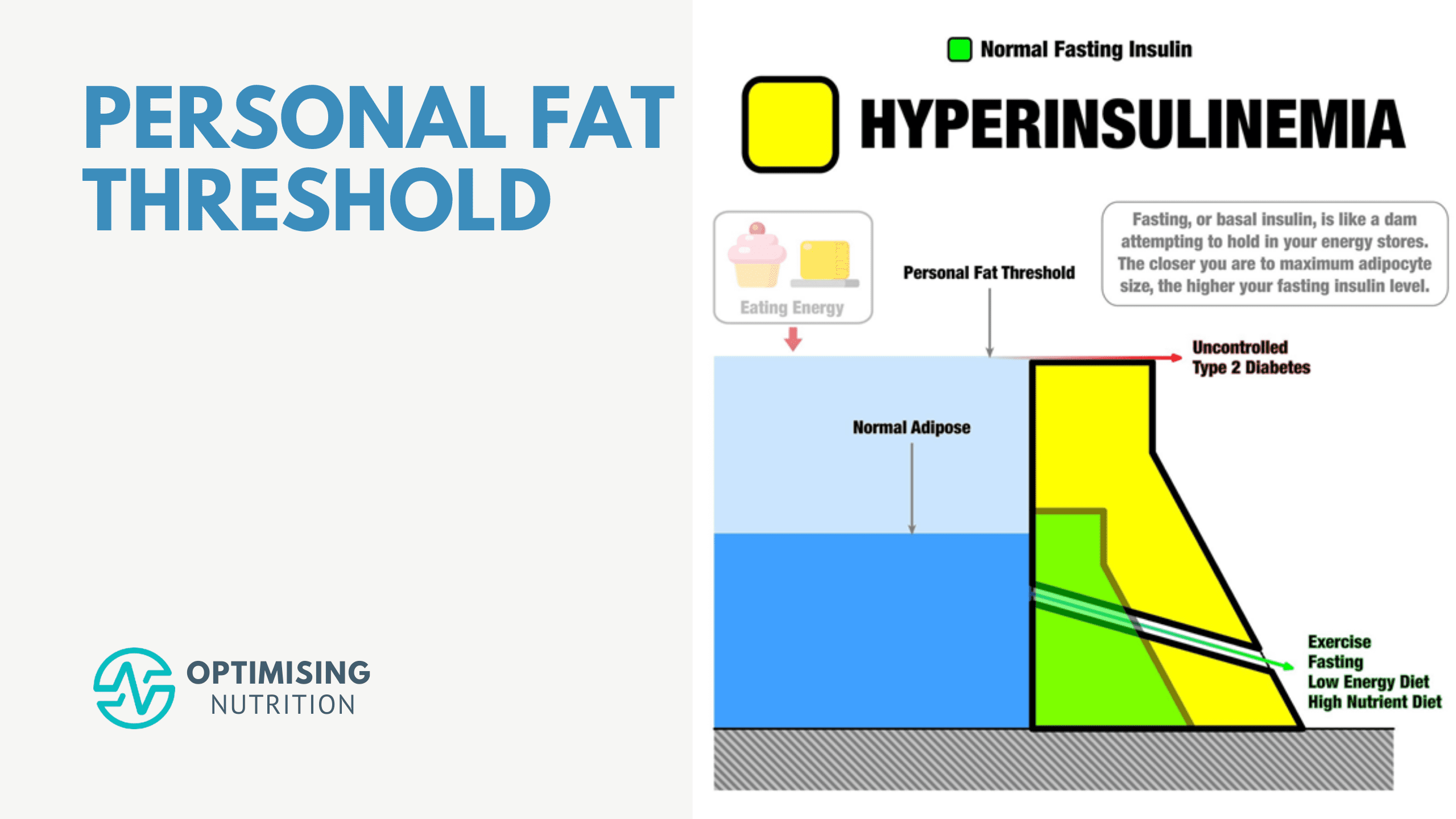
Your Personal Fat Threshold & High Insulin Levels
Explore the intricate relationship between insulin resistance and fat storage as you delve into understanding your personal fat threshold. Discover actionable steps to manage your weight and enhance metabolic health.