The keto diet craze has spawned countless products, recipe books, and a dedicated following, all built on the premise that more ketones equals more fat loss. However, it’s high time to debunk this mistaken belief.
In this article, we’ll take you on a journey through the fascinating world of ketosis, shedding light on the truth behind the ketogenic diet. We’ll explore the critical distinction between endogenous ketosis (ketosis from within your body) and exogenous ketosis (ketosis induced by external sources) and why it matters.
Prepare to be enlightened. Ketosis isn’t the singular answer to your fat loss goals. By the end of this article, you’ll understand how ketosis works, how to measure it effectively, and why it may not be the holy grail of weight loss you once thought it was.
Let’s uncover the real secrets to a healthier you.
- What is Ketosis, and When Does It Occur?
- What Does It Mean to Have High Blood Ketones?
- What Are ‘Peetones’?
- Breath Acetone
- The Personal Fat Threshold
- The Glucose:Ketone Index (GKI)
- The Glucose:Acetone Index
- Should You Measure Ketones?
- Is There a Specific Number That Indicates I Am in ‘Fat-Burning Mode’?
- Summary
What is Ketosis, and When Does It Occur?
Ketones are produced by the liver when fat is broken down. This fat can come either from your body or your diet.
While ketosis can be a side effect of fat loss, it is not the cause of fat loss, and it does not make your body burns its own energy stores.
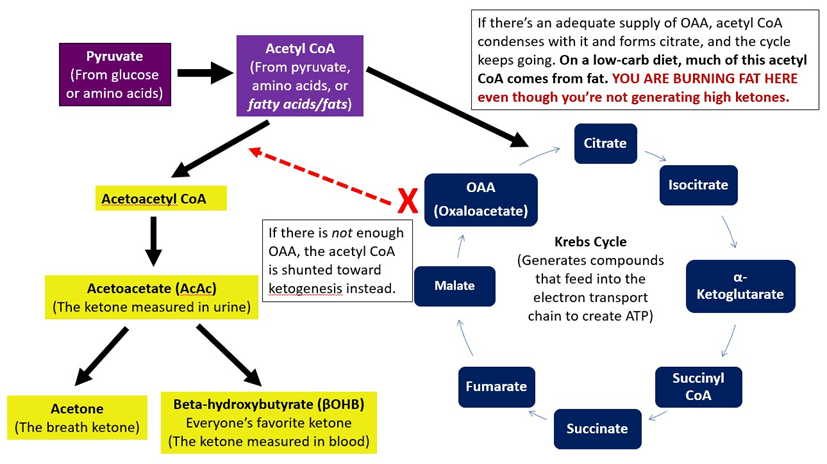
Your body typically burns fat in the citric acid cycle, but it requires oxaloacetate from carbs or protein. Ketosis is simply an alternative metabolic pathway that your body can use when there is less dietary oxaloacetate from carbs or protein to burn fat via the citric acid cycle. When carbs and protein are low, the fat that can’t be oxidised in the citric acid cycle is oxidised via ketosis.
The image below, created by certified nutrition specialist and author Amy Berger, demonstrates this graphically. On the right, we have the default process. On the left, we have ketosis, which occurs when there is inadequate oxaloacetate.
To quote my friend Mike Julian:
Ketones result anytime the citric acid cycle (TCA) in liver mitochondria encounters more acetyl-CoA than it can handle. This is a situation of relativity. However, as it can occur in two ways:
You can provide more acetyl-CoA to the liver TCA cycle by ingesting something like MCT oil or coconut oil. This surplus acetyl-CoA will exceed the TCA cycle’s capacity, resulting in the balance being shunted towards the ketogenesis pathway. This will trigger ketogenesis even in the presence of carbohydrates.
But ketosis can also occur when we restrict carbohydrates or skip meals. In this case, the sharp decline in carbohydrates and decrease in liver glycogen creates a situation in which gluconeogenesis becomes prominent.
The very act of gluconeogenesis depletes the liver mitochondrial TCA cycle of oxaloacetate because it is donated to the process of gluconeogenesis. The TCA cycle can no longer operate at its previously higher capacity with less available oxaloacetate. Now, incoming acetyl-CoA will overwhelm the liver TCA cycle capacity more easily, resulting in the surplus acetyl-CoA being shunted off towards the ketogenesis pathway.
In a low-carb setting, ketogenesis is a by-product of gluconeogenesis. Or, more broadly, ketogenesis is the result of the ratio of acetyl-CoA to the availability of oxaloacetate. Any time you create a situation where acetyl-CoA is higher than available oxaloacetate in the liver, the TCA cycle can facilitate ketogenesis.
This backup metabolic pathway has helped humans survive many a famine. We see beneficial upregulations in mitochondrial biogenesis, sirtuins, autophagy, and the NAD+:NADH ratio when our energy levels are low. Our body goes into repair mode to ensure survival, and we switch over to burning body fat.
Many glorify ketosis as a magical state with many benefits. However, we often miss the fact that most benefits are NOT necessarily due to the ketones themselves but rather the energy deficit associated with endogenous ketosis when your body is using the fat on your body for energy.
What Does It Mean to Have High Blood Ketones?
Ketones take several different forms and roles in your body. As shown in the figure below, the energy that cannot be burned in the citric acid cycle enters as acetyl-CoA, where it is converted to ketones as acetoacetate.
If your NADH:NAD+ ratio is high from excess stored energy in your body, ketones will be stored as BHB in your blood. Later, your body might have to convert BHB back to acetoacetate before it can be used for energy if required.
You can think of BHB as the storage and transport form of ketones in your body. The BHB ketones that you measure on your blood ketone meter tell you how much energy you have stored as ketones in your bloodstream. Unfortunately, the amount of BHB in your blood doesn’t tell you whether you are using them for fuel or just filling your bloodstream with more energy.
We can liken the relationship of acetoacetate and BHB to glucose in the bloodstream and glycogen stored in the liver. Acetoacetate and glucose are burned in your body, while BHB and glycogen are the fuel storage forms that need to be converted back to the active forms used in your body.
What Are ‘Peetones’?
Unfortunately, it’s hard to measure acetoacetate levels, the active form of ketones, in your blood.
When someone is in the early stages of fasting or goes on a ‘ketogenic diet’, they can measure acetoacetate in their urine. These are sometimes referred to as ‘peetones’.
Most people deem acetoacetate in the urine to be a poor measure of ketosis because they tend to reduce to undetectable levels after a few days or weeks. People new to a ‘ketogenic way of eating’ often get confused and think they’ve done something wrong when they can no longer measure ketones in their urine.
However, the reduction in ketones may be because either:
- the body quickly adapts to using acetoacetate for energy, or
- with less oxaloacetate available and less reliance on ketosis to produce energy, we revert to burning fat more efficiently in the citric acid cycle.
Similar to high levels of BHB in the blood, spilling acetoacetate into the urine is not a sign that you are using ketones for energy. Instead, it indicates that you are making more ketones than your body can use.
It makes sense that our bodies would adapt to use all available energy rather than wasting it for too long.
Breath Acetone
While it is hard to measure the level of acetoacetate in your body, we can measure the acetone produced as a by-product when it oxidises to acetoacetate. This is commonly known as ‘breath acetone’, BrAce, or ‘breath ketones’.
Measuring BHB has limited usefulness because we are measuring stored ketones. However, measuring breath acetone can help us determine whether we are using ketones (acetoacetate) for energy.
The Personal Fat Threshold
Some people think of diabetes as a disease of glucose intolerance. Hence, the solution is simply to avoid carbohydrates. But, thanks to Professor Roy Taylor’s excellent work on the Personal Fat Threshold, we have come to understand that diabetes is related more to an inability to store excess energy from your diet as body fat.
Once your body fat stores become full, and you exceed your Personal Fat ThresholdPersonal Fat Threshold. Then, any extra energy from your diet is released into your bloodstream as high glucose levels, ketones, and free fatty acids are stored in your vital organs.
While most people become obese before developing full-blown Type 2 Diabetes, this is not always the case. For reasons that we don’t fully understand that are likely related to genetics, race, inflammation, toxins and diet, some people can exceed their PersonalFat Threshold while still appearing relatively lean.
On the other extreme, some people can remain insulin-sensitive with healthy blood glucose levels even while putting on massive amounts of weight. The most insulin sensitive people can become very large before their bodies lose the ability to store excess energy from their diet as adipose tissue.
Once you can drain the excess energy from your body, your fat stores will be able to do their job efficiently. Excess energy will no longer back up and overflow into your blood. At this point, you will likely see lower levels of glucose, ketones, and free fatty acids in your blood.
Continuing to add more energy from dietary fat or exogenous ketones in the pursuit of higher ketones will only worsen the root cause of energy toxicity and commonly associated metabolic diseases.
The Glucose:Ketone Index (GKI)
We know from the previous chapter that lower glucose levels are a good thing, and ketones may be beneficial (depending on the context).
- In the absence of carbs or protein from the diet during starvation, BHB ketones can nourish the brain through endogenous ketosis, stay alert and find food.
- If we are managing conditions like Alzheimer’s, epilepsy, or Parkinson’s, therapeutic ketosis via exogenous ketosis also appears to be beneficial.
- High ketones are not desirable if they are also accompanied by high blood glucose levels or free fatty acids. You are merely driving a high energy state in your body with lots of extra fuel.
One way to ensure we are not overloading our system with excess energy from our diet is to ensure that higher ketone levels are accompanied by lower glucose levels.
Professor Thomas Seyfried developed the glucose: ketone index (GKI) (see The Glucose Ketone Index Calculator: A Simple Tool to Assess Therapeutic Efficacy for Metabolic Management of Brain Cancer).
Seyfried advocates fasting for cancer patients and uses the GKI to track their metabolic health during fasting. As discussed in Optimal Nutrition for Cancer Management, excess glucose and the surplus of energy that is associated with obesity appear to drive cancer growth.
If insulin levels are not excessive, we would see higher BHB ketones during a fasting period as glucose levels decrease and ketone levels rise to make up for the energy deficit.
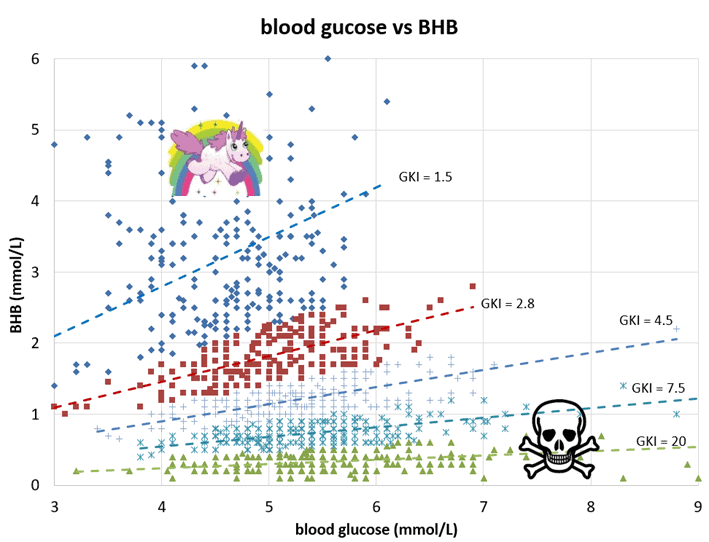
To understand what the GKI might look like in practice, I plotted more than 1,200 blood glucose versus ketone values using data supplied by Michel Lundell of Ketonix.
These values are divided into five groups based on their GKI value. If you were fasting, a lower GKI would be better; your blood glucose levels would be low, and your ketones would rise to supply the fuel necessary for your brain and vital organs.
The people with the worst metabolic health are represented by the green dots at the bottom of the chart where GKI = 20. These people have high blood glucose levels and low ketones, and their glucose values are 20 times that of their ketone values.
Most of the time, people will not get GKI values under 2.0 until they fast for a few days. The chart below shows what you could expect if you fasted for seven days based on my data combined with several others who tested their ketones and glucose during an extended fast.
However, the problem with the GKI again comes when people confuse exogenous ketones (from outside the body) and endogenous ketones (from within your body) or think they are equivalent.
Lately, the GKI has sparked interest in Ketoland, with many people chasing a lower GKI as a badge of honour. Rather than monitoring long-term fasting as designed, more people are combining fasting with high-fat eating to get lower GKI values.
Sadly, this is unlikely to lead to optimal body composition over the long term. Adding more low-satiety, nutrient-poor refined fats to keep GKI values low will exacerbate metabolic issues by driving energy toxicity.
The Glucose:Acetone Index
If you wanted to check if you were burning rather than storing fat using ketones, breath acetone (BrACe) might be a more useful measure of beneficial ketosis.
When the storage form of ketones BHB is converted to acetoacetate for energy, acetone is released as a by-product and can be measured by breath.
Acetone is a vapour similar to nail polish fumes that is released from acetoacetate. If you are releasing a high level of breath acetone, you may experience fruity-smelling breath or a metallic taste in your mouth.
You can measure BrAce to understand if you are using ketones rather than just storing them. Many people now seem to be showing more interest in breath acetone after noticing that it yields better outcomes in patients using ketosis therapeutically.
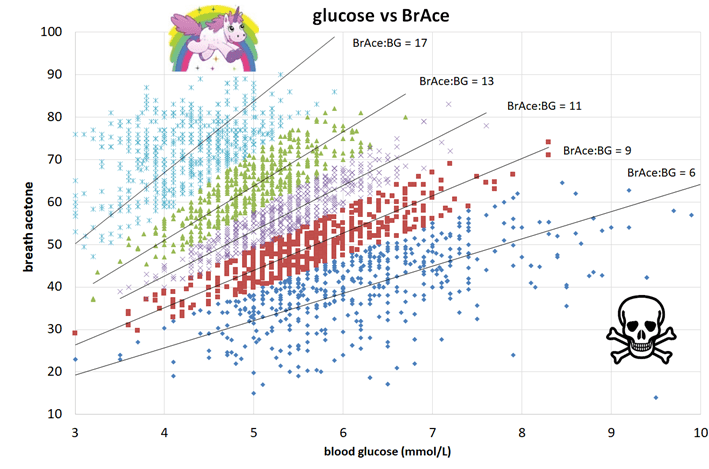
I plotted 2500 glucose and breath ketone readings in the chart below to better understand the relationship between breath acetone and blood glucose.
You can see from this chart there is a similar relationship between glucose and breath ketones as with blood ketones, but there is less scatter than with the GKI chart. Blood glucose and breath acetone are correlated more closely than blood ketones.
It’s hard to have high breath acetone with high blood glucose levels. You can’t manipulate the system by forcing in more and more dietary fat or exogenous ketones the same way you can with BHB.
The optimal situation is to have lower blood glucose levels with a significant amount of breath acetone in your system. This would indicate that you are producing ketones without consuming excess energy.
You’ll probably fall in the purple or green areas on the chart towards the top left if you have good metabolic health. If you reach a therapeutic level of ketosis or fast for extended periods, you will ideally fall in the upper left area that is green or light blue, with low glucose and high breath ketones.
Different breath ketone meters, unfortunately, use different units for BrAce, so it’s hard to standardise a good versus bad glucose:BrAce ratio. However, if you wanted to track glucose and breath acetone simultaneously, you would want to see the ratio increase over time. This would indicate that your glucose is dropping and that you are effectively oxidising ketones.
Should You Measure Ketones?
If you require therapeutic ketosis to manage conditions such as epilepsy, Alzheimer’s, or dementia, then it may be helpful to monitor ketones.
Given that BHB ketones are more a measure of the energy stored in your body and BrAce is more a measure of how well you’re using ketones for energy, BrAce may better indicate if you are utilising ketones for energy rather than storing them.
If you want to track your ketones and glucose, the glucose to breath acetone ratio will be the most useful thing you can measure. Over time, you want to see your breath acetone divided by your glucose increase as your metabolic health improves.
However, if you do not require therapeutic ketosis, simply monitoring glucose, weight, waist, and perhaps body fat will give you most of the information you require to ensure you are moving in the right direction.
Is There a Specific Number That Indicates I Am in ‘Fat-Burning Mode’?
The concept of a single magic number that indicates you are burning fat or in ‘fat-burning mode’ is alluring as measuring blood ketones does not tell you whether that fat is coming from the high-fat food you are eating or your body.
If your goal is body fat loss and improved metabolic health, tracking your blood glucose before eating is likely more useful. The best way to manage your pre-meal glucose value is to simply wait a bit longer to eat until your body has used up more of the glucose in your system. As your premeal blood glucose levels reduce, your body will progressively turn to burn more fat, particularly at rest.
Summary
- You don’t need to be ‘in ketosis’ or have elevated ketone levels to burn fat from your diet or body.
- Ketosis is an alternative pathway that your body uses to burn fat in the citric acid cycle when you don’t have enough carbs and protein available for energy production.
- When you eat enough carbohydrates or protein, you will be burning fat in the default citric acid cycle.
- If you eat a satiating diet that leads to an energy deficit with adequate protein, you may have lower ketones, but you will still be burning fat.
- Measuring blood ketones is of limited use to guide your dietary choices because it is hard to know whether the fat is coming from your body or your food.
- Low glucose with higher ketones (especially breath ketones) may be more beneficial to track improved metabolic health via helpful markers like the glucose: acetone index.
- Waking glucose and your waist to height ratio is an excellent indicator of insulin resistance.
- Monitoring blood sugar before you eat is more valuable to guide meal timing and ensure you are moving towards improved metabolic health.
Get your copy of Big Fat Keto Lies
I hope you’ve enjoyed this excerpt from Big Fat Keto Lies. You can get your copy of the full book here.
What the experts are saying about Big Fat Keto Lies

Get Big Fat Keto Lies!
Get your copy of Big Fat Keto Lies here.
Sample the Other Chapters of Big Fat Keto Lies
- Big Fat Keto Lies: Introduction
- A Brief History of the Low Carb and Keto Movement.
- Keto Lie #1: ‘Optimal ketosis’ is a Goal. More Ketones are Better. The Lie that Started the Keto Movement.
- Keto Lie #2: You Have to be ‘in Ketosis’ to Burn Fat.
- Keto Lie #3: You Should Eat More Fat to Burn More Body Fat.
- Keto Lie #4: Protein Should Be Avoided Due to Gluconeogenesis.
- Keto Lie #5: Fat is a ‘Free Food’ Because it Doesn’t Elicit an Insulin Response.
- Keto Lie #6: Food quality is Not Important. It’s All About Reducing Insulin and Avoiding Carbs.
- Keto Lie #7: Fasting for Longer is Better.
- Keto Lie #8: Insulin Toxicity is Enemy #1.
- Keto Lie #9: Calories Don’t Count.
- Keto Lie #10: Stable Blood Sugars Will Lead to Fat Loss.
- Keto Lie #11: You Should ‘Eat Fat to Satiety’ to Lose Body Fat.
- Keto Lie #12: If in Doubt, Keep Calm and Keto On.
- Resources











Certainly a deep dive. Thank you
Cheers!