This article unpacks the mechanisms of type 2 diabetes and sets out a road map to help you reverse type 2 diabetes and achieve optimal blood glucose, fat loss and long-term metabolic health.
Embarking on a journey towards reversing Type 2 diabetes might seem daunting, but what if the antidote lies right in our daily food choices? This article explores the compelling relationship between nutrition and diabetes, providing a roadmap to harness the power of specific foods in achieving optimal blood glucose levels and promoting long-term metabolic health.
Uncover a wealth of insights that aim to demystify the complexities surrounding diabetes, offering a beacon of hope for those eager to take control of their health through a well-informed dietary approach.
Your path to a healthier, diabetes-free life is just a read away.
- Is type 2 diabetes reversible?
- Medical Disclaimer
- Type 1 vs type 2 diabetes
- The commonalities
- The differences
- Diabulimia and the Carbohydrate Insulin Hypothesis
- When can you claim you have reversed diabetes?
- Your multiple fuel storage tanks
- 1. Alcohol
- 2. Ketones
- 3. Protein
- 4. Carbohydrate
- 5. Fat
- Personal fat threshold
- TOFI vs. metabolically healthy obese
- What changed?
- Will fasting reverse your type 2 diabetes?
- Do I need to worry about ketones?
- What about exogenous ketones?
- Micronutrients
- Should I avoid protein?
- But isn’t protein insulinogenic?
- Muscle gain and improving insulin sensitivity
- Reverse type 2 diabetes – progression stages
- Food choices
- Further reading
Is type 2 diabetes reversible?
According to the American Diabetes Association, diabetes is a progressive disease.
Apparently, there’s not much you can do. You might as well accept it and just take the medications.
According to the official story, over time you’ll probably just get fatter, experience a range of debilitating complications, and most likely have a heart attack and die early.
Sounds like a pretty depressing prognosis!
Thankfully, it does not have to be this way.
The solution is not complex, but it’s not easy and it doesn’t come in a pill.
It will take some hard work and you will need to be motivated.
It also requires some ongoing refinement and adjustment as you progress towards optimal health.
It is not a one-size-fits-all solution.
This article will give you a map to show you how to get there.
Medical Disclaimer
I’m an engineer, not a doctor.
This article will help you
- to understand the flow of fuel in your body,
- how to reduce your requirement for insulin, and
- how to manage micronutrients to maximise mitochondrial function thereby giving you the best chance of achieving excellent blood sugar control and a long, happy and healthy life.
If you are looking for information about drugs to manage your diabetes you should consult your doctor.
Type 1 vs type 2 diabetes
Type 1 and type 2 diabetes are similar but different.
While we can learn a lot from people who manage type 1 diabetes well, it is also critical to understand the differences between type 1 and type 2.
Once we understand the differences we will be better equipped to understand what to do when an approach that is helpful for type 1 (e.g. a keto or low carb diet) stops working.
The commonalities
- Both type 1 and type 2 are characterised by a relative insulin insufficiency. That is, people with diabetes don’t have enough insulin to stop stored energy being released into their bloodstream.
- Diabetes is a condition of excess energy in your bloodstream. While we usually focus on glucose, this excess energy can also take the form of blood ketones and free fatty acids.
- Both type 1 and type 2 diabetes can be managed with diet. Reducing the carbohydrates in your diet can help to decrease the need for insulin injections and other medications (which seem to be costing us more and more these days).
A diet with less refined carbohydrates will help stabilise your blood sugars and thus manage many of the symptoms of your disease.
However, it is not a cure for either type 1 or type 2 diabetes. A reduced carbohydrate diet is potentially just the start of your journey.
The differences
There is no known cure for type 1. The pancreas simply doesn’t produce enough insulin, so someone with type 1 diabetes needs to inject insulin to meet the shortfall.
In type 2 diabetes, the pancreas is still able to make insulin, but not enough to hold back the buildup of energy stored in your body, so it overflows into your bloodstream.
Though not recommended, someone with type 1 diabetes could choose to stop taking insulin. This will cause their stored energy to quickly be released into their bloodstream in an uncontrolled manner. Without insulin, they will basically melt away in a matter of weeks or days.
The photos below show children with type 1 diabetes from a century ago, before and after insulin injection.
Thankfully, now with the availability of insulin, the condition is usually addressed before it gets so bad.
Diabulimia and the Carbohydrate Insulin Hypothesis
Some type 1s intentionally choose to under-dose their insulin and run their blood sugars high in order to lose weight. This is a very dangerous eating disorder (known as diabulimia) that leads to high blood glucose, high blood triglycerides, high blood ketones as well as muscle loss.
While it’s my wife who has type 1 diabetes, I used to believe that I could manipulate my diet to reduce the insulin load of the food I ate to induce a sort of diabulimia in myself.
While it might sound crazy, this belief that calories from fat won’t make you fat is actually quite widespread and is commonly known as the Carbohydrate Insulin Hypothesis of Obesity.
Unfortunately, I just ended up overeating refined dietary fat (which I now understand is not satiating) and gained a lot of unwanted body fat.
Reducing your carbohydrate intake will reduce your requirement for insulin and stabilise your blood sugars. But, unless you have type 1 diabetes, you will always have enough insulin to store the excess energy from your diet.
People with type 2 can still have very high fasting insulin levels on a high-fat ketogenic diet in spite of undertaking extended fasts on a regular basis.
Injected (exogenous) insulin will slow lipolysis and make you hungry. But, left to its own devices, your body is highly efficient. Your pancreas will not raise insulin more than necessary to hold back your body fat in storage while it uses up the energy coming in via your mouth!
While many of us would like to believe that switching to a high-fat diet will cause our fat to melt away (a bit like an uncontrolled type 1 diabetic), it doesn’t actually work in practice.
Diabetes reversal is ultimately an issue of energy balance. You need to find a way to get below your Personal Fat Threshold to the point that your body fat has some capacity so it can do its job as a buffer for excess energy from your diet.
To truly reverse diabetes, we need to sustainably reduce our energy intake. However, it is critical to ensure you get adequate nutrients to promote satiety and prevent rebound binging that often accompanies weight loss.
When can you claim you have reversed diabetes?
Your doctor will diagnose you with prediabetes if you have an HbA1c greater than 6.0% and type 2 diabetes once your HbA1c hits 6.5% and above. Official cut-offs for blood sugar and HBA1c are shown in the table below.
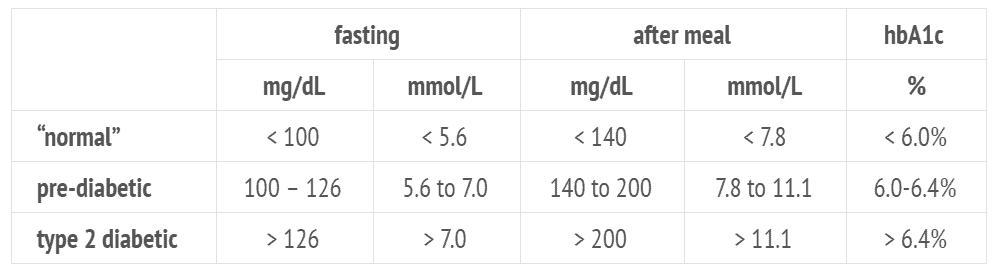
However, optimal blood sugars are significantly lower than what is usually considered to be “normal”.
As the charts below show, your lowest risk of heart disease, stroke, cardiovascular disease, and death from any cause tends to correlate with a Hba1c closer to 5.0%.
While you can manage some of the symptoms with antidiabetic medications, it does not necessarily reduce your risk of complications from the underlying disease. In fact, some of the medications may actually exacerbate the complications, stop you from being able to access your body fat for fuel, increase your appetite and drive you to eat more.
If you aim for optimal health rather than “normal”, you should have a HbA1c of less than 5.4%, with the ability to eat a range of foods without experiencing elevated blood sugars to claim to be “cured legitimately”.

While it is possible to reverse type 2 diabetes, it is much better to take action before your pancreatic beta cells burn out.
Your multiple fuel storage tanks
Your body is an amazing machine!
Humans have learned to adapt and thrive on a range of different fuel sources in a range of environments (e.g. summer/winter and Arctic/tropics).
We store the different fuels we can use in separate but interconnected compartments.
The graphic below helps to explain the oxidative priority and dietary-induced thermogenesis that correspond to the different fuel sources.
All of these fuel tanks have to be depleted to some extent before we get to the point where we can use up our body fat and reverse type 2 diabetes.
If you want to see your abs, reduce blood sugars, reduce your insulin levels, reverse your diabetes and avoid the raft of modern diseases that are bankrupting our Western civilisation, you need to find a way to sustainably reduce the amount of fuel we stack up in front of our body fat, which gets burned last.
Only once we restore the capacity in our body fat to absorb extra energy will it stop overflowing into our bloodstream (i.e. type 2 diabetes).
To understand how we can actively manage our fuel tanks, we need to look at each of the fuels a bit closer.
1. Alcohol
The body can use alcohol for fuel. It burns quickly and gives us energy (7 calories per gram).
You probably know that if you drink enough of it, you feel warm, “buzzed” and get a red face as the body tries to burn it off.
Someone who is drunk might have about 30 calories worth of alcohol in the bloodstream. However, other than a very small amount in the blood (about 30 calories worth), the body doesn’t have anywhere to store alcohol, so we have to use it first before everything else.
2. Ketones
Ketones are another fuel source that the body can use. The body produces ketones naturally when there aren’t a lot of carbs and protein available. Ketones ensure we can continue to fuel our brain and heart in times of starvation.
More recently, chemists have also worked out how to make exogenous ketones.
We have some capacity to store ketones as beta-hydroxybutyrate in our bloodstream, but not a lot, probably up to about 30 calories worth (i.e. the same amount as alcohol).
Similar to alcohol, when ketones are elevated (particularly from consuming exogenous ketones), your body will prioritise burning them to return to healthy blood ketone levels.
Your body doesn’t want the level of ketones in your bloodstream to rise too high (we call this ketoacidosis), so your pancreas raises insulin to hold everything else back in storage until the ketones in your bloodstream return back to normal levels.
3. Protein
Protein is critical to many of the functions in your body. The body has a strong appetite for adequate protein to maintain your muscles and vital organs.
However, once we get enough protein, our appetite switches off because excess protein is a poor fuel source. We start looking around for energy from fat or carbs.
We lose 25% of the energy from protein, converting it to ATP to be burned in our mitochondria.
We do have some capacity to store protein, but not a lot. If we do consume too much protein, the body prioritises burning it off before carbs and fat so we don’t end up with too much of it in our bloodstream.
The key thing to note here is that while excess protein does need to be burned off as a priority, protein also has a stronger satiety response relative to fat and/or carbs.
We find it hard to overeat protein because we can’t store much of it as it’s hard to convert to energy.
As shown in the chart below from our analysis of half a million days of food logging, prioritising protein tends to help us eat less overall.
Our more recent analysis of 25,000 days of data from people using the Nutrient Optimiser shows a similar trend.
4. Carbohydrate
We can store about a day’s worth of energy as glycogen (the storage form of glucose) in our bloodstream, liver and muscles.
Similar to the other upstream fuels, when you get too much glucose in your bloodstream, your pancreas will raise insulin to send a signal to your liver to shut off the flow of fat from storage until your blood glucose levels return to normal.
High levels of carbohydrates in your bloodstream mean that you are not able to burn fat. We see this on the surface of type 2 diabetes – elevated blood sugar levels.
You won’t burn the body fat until you deplete the glucose in your system.
Carbohydrates are a more efficient fuel source than protein, and we only lose 8% in the conversion to ATP.
Your appetite will drive to consume more carbohydrates when they are available until your glycogen stores are full.
Elevated blood sugars are a clear sign that your carbohydrate tank is full (glucose in the bloodstream and glycogen in the liver and muscles). A reduced carbohydrate diet is a no-brainer for people with diabetes.
The Nutrient Optimiser Smart Macros Algorithm helps you to titrate down your carbohydrate intake until your blood sugars stabilise.
5. Fat
You have a significant amount of storage capacity for fat in your bloodstream to carry energy around your body (i.e. cholesterol, HDL, LDL etc).
The body loves to burn and store fat. Only about 3% is lost in the conversion to ATP and we don’t seem to need as much insulin to hold our fat in storage.
Because fat is so energy-dense (9 calories per gram versus 4 for carbohydrate and protein) it is great for storage; therefore the body ensures that the other fuel sources are burned off first, and saves the fat for storage for a future time when food is harder to find.
You have a virtually unlimited capacity to store fat in your adipose tissue, at least until you reach your Personal Fat Threshold.
Personal fat threshold
Personal Fat Threshold is a term coined by Professor Roy Taylor, who observed that:
- although most people become diabetic once they have gained a significant amount of body fat,
- some people develop diabetes with a lower level of body fat and
- others can continue to put on massive levels of body fat while maintaining excellent blood sugar levels.
Your Personal Fat Threshold is when your body fat (adipose tissue) becomes full and inflamed and can no longer store more energy efficiently.
Your pancreas has to ramp up insulin production to hold back your fat in storage. Any excess energy eaten gets stored as fat in other places, such as your vital organs, which are now more ‘insulin sensitive’ than your overdue fat stores.
At this point, the fuel flow in your body basically backs up like a traffic jam with too many vehicles coming from too many different directions, all at the same time.
If your adipose tissue is not acting as a buffer the way it’s meant to, the fat in your bloodstream will increase, the glucose in your blood will increase, and your kidneys will try to clear the protein from your bloodstream because you can’t burn it off anymore. You may even see elevated blood ketones.
TOFI vs. metabolically healthy obese
At one extreme, people cannot build up a lot of body fat before becoming diabetic.
These people are sometimes known as TOFI (thin on the outside, fat on the inside). Excess energy that can’t be stored in their subcutaneous fat stores overflows into their bloodstream and is stored in their vital organs.
The DEXA scan below shows the difference between someone who holds fat around their organs (left) and someone who holds their fat under their skin in subcutaneous fat stores (right). The person on the right still has plenty of room for their fat stores to expand before spilling over into their vital organs.
At the extreme end of the TOFI scale, we have someone like Lizzie Velásquez (shown below), who was born with a rare congenital disease called Marfanoid-progeroid-lipodystrophy syndrome which means that she is only able to store a little bit of fat in her subcutaneous adipose tissue.
The guy on the left in the photo below can continue to store a massive amount of energy in his adipose tissue while the guy on the right starts to jam excess energy into his organs in his abdomen earlier.
We don’t yet fully understand why different people have different capacities to store fat. It could be partly genetic, toxin-related, stress, sleep, cortisol etc. or likely a mixture of all of these and more.
Excitingly, Professor Taylor also showed that as we start to lose body fat, the fat in our vital organs and bloodstream is the first to go. If you can reduce your body fat below your Personal Fat Threshold, you will be on the road to reversing your diabetes!
If you already have diabetes, the way to determine your Personal Fat Threshold is to lose weight while tracking your blood sugars and body fat percentage. The body fat percentage at which your blood sugars normalise is your Personal Fat Threshold.
To go back to our roundabout analogy, the secret to managing your body fat and reducing fuel congestion in your bloodstream is to ensure that you aren’t simultaneously pouring in fuel from all sources.
In days gone by, there would usually be a single dominant fuel source depending on your location and season, while the others were relatively scarce (i.e. protein+fat in winter, protein in spring, carbs in summer and carbs+fat only in autumn).
However, as we will see below, our modern food environment has created a unique situation where we can constantly fill all fuel tanks at once. It’s no wonder we rarely get to burn our body fat which is only used once all the other fuel sources are used up!
What changed?
It’s no secret that we seem to be getting sicker and fatter lately.
But it hasn’t always been this way.
What changed?
Over the past fifty years or so, the proportion of our food that is some combination of starch+fat+sugar has increased markedly. While the foods with this combination are rare in nature, they now dominate our restaurants, grocery aisles and convenience meals we eat at home.
The increase in energy in our food system has largely come from the increased use of added fats and oils (e.g. soy, corn, canola) together with cereals and grains. You can see in the chart below that added sugars increased until 1999 but have mostly come back down while all the other food groups have stayed fairly stable.
The combination of carb+fat in foods used to only be available in autumn to help animals (including us) prepare for the coming winter.
The only naturally occurring foods containing a similar mix of carbs and fat are breast milk (which helps babies quickly grow into children) and acorns (which fatten squirrels for winter).
The creation of chemical fertilisers in the 1930s enabled us to grow more food more quickly. Today, foods with this fat+carb combination are everywhere. They tend to be “comfort foods” for which we have no off switch. We find it virtually impossible to resist these foods when they are available.
You shouldn’t really feel too guilty about this. It’s not really a matter of willpower, self-restraint or moral weakness; you’re just programmed to eat these foods when they are available. And once you start, our appetite ensures we don’t stop until we are stuffed!
The chart below shows that lab rats eat more when accessing fat+carb foods. This food combination tends to cause a binge instinct (or hyperphagia) by signalling that it’s autumn and we must eat to prepare for winter NOW!
The recommendation to ‘eat less, move more’ is futile unless you change the quality of your food. If you’re surrounded by processed junk food, your appetite will generally win out and ensure you eat to refill your fat stores.
Filling both your carbohydrate and fat fuel tank at the same time is a surefire way to ensure that you will never need to burn your own body fat.
The chart below shows that over the past 100 years, the carbs and fat in our diet have trended towards similar levels in percentage terms as our food processing has made things more refined to fine-tune manufactured foods to give us what we want.

While the amount of available carbohydrates has gone down and then back up, fat from refined vegetable oils has been steadily on the rise over the past century.
This combination of carbs and fat has enabled us to consume more energy which appears to have driven the obesity epidemic. It’s not simply a matter of calories in and calories out, but that the foods we eat are driving us to eat more.
Will fasting reverse your type 2 diabetes?
Fasting is a great way to reduce your energy intake, use up some stored fat and reduce insulin levels. But it’s important to do it with a goal in mind.
- If you have elevated blood sugars, use your glucose meter to help guide your meal timing and extend the time between meals (see How to use your blood sugar meter as a fuel gauge).
- Once your blood sugars stabilise, you can use your weight on the scale to guide your fasting routine (see How to use your bathroom scale as a fuel gauge).
The problem with fasting often comes with re-feeding. It’s hard for many people to make wise food choices when they are really hungry. We often optimise food to refuel quickly, which usually involves high levels of fat and possibly carbs, and usually not enough protein.
“Every fool can fast, but only the wise man knows how to break a fast.”
George Bernard Shaw
Without modifying food quality, our appetite often does a great job of ensuring we eat back the same energy that we missed out on while fasting.
There is a real risk that regular long-term fasts will diminish food quality. It’s difficult to consume the protein and other nutrients you need in a narrow window of time, and it’s much easier to reach for more energy-dense food combinations.
Our recent analysis of half a million days of MyFitnessPal data suggests that eating breakfast and lunch is the best way to keep your energy intake down over the long term (see How many times should I eat a day to lose weight?).
It seems you will have a much better chance of eating less across the day if you prioritise breakfast (see Breakfast Like a king, Lunch Like a prince and dinner like a pauper).
And while you’re at it, making sure you get a substantial amount of protein at breakfast will help you eat less across the rest of the day.
Do I need to worry about ketones?
No. You don’t need to focus on elevated ketones to lose weight or reverse your diabetes.
Your body is always burning fat to some degree, regardless of the ketones you can measure in your blood.
As shown in the chart below, our recent analysis of half a million days of MyFitnessPal data suggests that you have a good chance of achieving satiety and eating less if you consume meals that have less than 30% carbohydrates. This enables you to avoid the hyper-palatable danger zone that occurs when we consume meals with 30 – 55% carbs.
When you are burning your own body fat, you will be producing ketones. Most of the positive benefits occur (in addition to just fat loss) when you are burning your own body fat.
However, as we push to a very low-carb diet with more refined fat and less protein, we will end up with exogenous ketosis (i.e. ketones made from the fat in your food that you just ate).
While a high-fat diet may be beneficial in managing chronic conditions such as epilepsy, Alzheimer’s or dementia, if your goal is weight loss or management of diabetes, you don’t need to chase higher ketone numbers.
While some people suggest that you should ‘eat fat to satiety’ or that you need to ‘eat fat to lose fat’, it seems that refined dietary fat (i.e. separated from protein) has a very low satiety on a calorie-for-calorie basis.
Ketogenic diet proponents often advocate for a moderate protein diet to ensure ketones remain elevated, but it appears that refined fat actually has a very poor satiety response once you remove protein.
Fat may make you feel full quickly because it has a high energy density. However, you will consume a lot more energy to feel full than you would have if you made more satiating food choices.
Many people get caught up believing that ketones equate to fat loss or hold some magical power and continue to chase elevated ketones with a high-fat diet that leads to fat gain and worsening insulin resistance.
The reality is that it’s hard to separate the benefits of ketones from simply eating less.
The chart below shows a compilation of 3000 ketones+blood glucose readings. People with optimal blood sugar control do not have elevated ketone levels, even on a low-carb or ketogenic diet.
Once your fat stores are no longer overfull, the fuel will no longer be backing up in your body. Your blood sugars, triglycerides and ketones will all decrease.
While you will be able to access ketones easily when food is scarce, you don’t need large amounts of them in your bloodstream.
The recently released two-year Virta study results showed that people on a ketogenic diet under the supervision of expert doctors and nutritionists initially experienced a bump in blood ketone values. However, over time they settled back down.
We also saw a similar phenomenon in our first Nutrient Optimiser Challenge, with ketones rising initially and then settling back down as people continued to lose weight.
While ketones seem to take a little longer to respond in people who identified as insulin-resistant, everyone seemed to lose weight at around the same rate.
What about exogenous ketones?
Over the last few years, we have seen an explosion in the popularity of exogenous ketones, which enable you to top up the ketones in your bloodstream as well.

This really is an unnatural scenario. Until now, ketones were only available when carbs and protein were virtually unavailable.
Topping up your ketone stores while also eating carbs, fat, protein or alcohol is pretty much the most effective way to ensure that your body fat is never called on.
Micronutrients
Micronutrients are critical to support healthy mitochondrial function to ensure you can use the energy you consume.
In addition to managing your macronutrient balance, ensuring you have adequate micronutrients in your diet is essential, especially if you are trying to lose weight by restricting energy and want to reduce your cravings.
When it comes to diabetes management, there are a number of key micronutrients that you should keep an eye on to maximise your chance of recovery.
- Vitamin B12 deficiency is common in people with diabetes because metformin depletes B12.
- Niacin preserves beta-cell function.
- Vitamin D lowers your risk of type 1 and type 2 diabetes and suppresses inflammation of pancreatic beta cells.
- Vitamin E provides protection against diabetes by protecting pancreatic B-cells from oxidative stress-induced damage.
- Vitamin C lowers HbA1c, fasting, and post-meal glucose in people with type 1 diabetes.
- Inositol may be effective in treating diabetic neuropathy.
- Carnitine reduces and even prevents pain from diabetic neuropathy and improves insulin sensitivity by increasing glucose uptake and storage.
- Glutamine stimulates GLP-1, which regulates insulin secretion after meals and improves insulin signalling and sensitivity.
- Coenzyme Q10 protects kidneys from diabetes-related damage and improves glycemic control in people with type 2 diabetes.
- Lipoic Acid enhances glucose uptake in skeletal muscle, improves glucose tolerance and is very effective in the treatment of diabetic neuropathy.
- Zinc is needed for the synthesis and secretion of insulin and protects the B-cells from damage.
- Magnesium deficiency reduces insulin sensitivity and exacerbates foot ulcers in people with diabetes.
- Biotin stimulates glucose-induced insulin secretion in pancreatic B-cells and can improve glycemic control.
- Chromium helps insulin attach to cell receptors increasing uptake into the cell. A deficiency of chromium can lead to insulin resistance.
While you could purchase all these supplements in bottles, the ideal approach is to do everything you can to get these nutrients from whole foods and use supplements only if necessary to fill any remaining gaps.
The Nutrient Optimiser will help you identify foods and meals that provide more of the nutrients you are currently not getting enough of.
As shown in the chart below, nutrient-dense foods are also typically more satiating (see full Tableau version here).

Should I avoid protein?
I used to believe that protein would increase insulin and slow fat burning. However, I now understand that protein actually maximises satiety, helps to manage appetite and reverse diabetes.
As shown in the chart below, foods with more protein and fibre are the most effective way to shut down your appetite.
The average American is consuming 12% protein which aligns with the lowest satiety and greatest likelihood of overeating.
Our appetite switches off once we get enough protein because protein is hard to convert to ATP, and our body has limited storage capacity.
By contrast, we can store a lot more carbs or fat, and the body will happily keep consuming carb+fat foods if they are available.
For most people, appetite will be a good guide for how much protein they need.
However, if you’re looking to lose weight, prioritising foods that provide a higher proportion of their energy from protein can help to improve satiety while decreasing body fat and blood glucose levels by not filling up those fuel tanks.
But isn’t protein insulinogenic?
Protein requires more insulin than fat (at least in the short term), so some people worry about ‘too much protein’ because it will ‘kick you out of ketosis’.
But the reality is that foods with more protein tend to lower insulin requirements because they displace carbohydrates and help you eat less overall.
If you’re injecting insulin, then it’s useful to understand how much insulin you will need to ‘cover’ your protein to keep your blood sugars stable; however, if you are trying to lose weight and/or manage type 2 diabetes ‘too much protein’ is not really a thing.
More protein is one of the factors in food that has a positive effect on satiety (along with a lower energy density and more fibre) will help you manage your appetite and enable you to eat less without excessive willpower. This will, in turn, enable body fat to flow out of storage and allow your basal insulin levels to decrease over time.
While it can be useful to monitor your blood glucose (you want to see the number trending down) or your breath ketones (you may want to see them higher to demonstrate you are burning fat), it’s much harder to make sense of your blood ketones.
Whatever you do, don’t go adding refined dietary fat in an effort to chase elevated blood ketone levels if you are hoping to lose weight!
Muscle gain and improving insulin sensitivity
Muscle burns fat and glucose, and hence important for people with diabetes.
The risk when losing weight, is that you lose a lot of muscle which will cause your metabolic rate to plummet unnecessarily.
If you have limited muscle mass, you will struggle to burn the energy from the fuel you eat. You will have to keep winding your calorie intake down to unsustainably low levels to continue to lose weight.
If you are losing weight, it is important to ensure you lose more fat than lean muscle mass.
The Nutrient Optimiser Smart Macros algorithm will help you keep an eye on your muscle mass loss rate vs. fat loss and suggest you increase your protein intake if you are losing more muscle than fat.
Of course, it’s also important to make sure you are maximising your muscle-building with physical activity at the same time.
Reverse type 2 diabetes – progression stages
So to recap, reversal of diabetes (rather than symptom management) requires you to lose enough body fat to return below your Personal Fat Threshold. Your body fat, which is no longer overfull, will act as a buffer for the food you eat so the excess energy from your food doesn’t overflow in your bloodstream.
You want reduced body fat while retaining lean muscle mass so you not only continue to look healthy on the outside, but so your metabolic rate doesn’t plummet.
Reversal of diabetes can be a long-term process that may require multiple changes and refinements in the dietary approach. Most people don’t switch from a hyperpalatable junk food diet to a high-satiety nutrient-dense diet overnight. It takes time to build new habits progressively.
To minimise the confusion and to help you take the most direct route possible towards optimal health, the Nutrient Optimiser platform guides you through the various stages with continual refinements to your macro targets and food choices based on your blood sugar levels, weight and % body fat levels until you achieve your goal.
The chart below shows that managing blood sugars and fat loss is not necessarily correlated (see interactive Tableau version here).
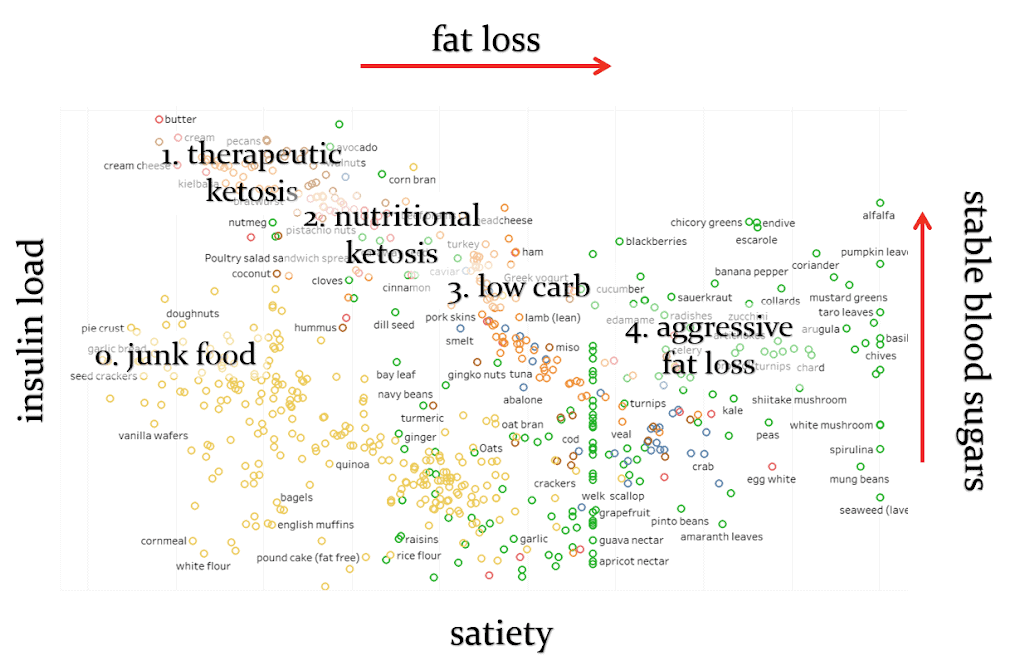
The Nutrient Optimiser will initially help you focus on stabilising your blood sugars via a lower insulin load diet. But then, as your blood sugars stabilise you can start to focus on more nutrient-dense high-satiety foods that will help you to lose body fat and move towards actual diabetes reversal.
Food choices
One component of the Nutrient Optimiser system is the optimised food lists and meals to help you dial in your diet to initially stabilise blood sugars and then progress towards fat loss while retaining your muscles.
We understand that most people don’t want to track their food, but if you are able to check what you are eating occasionally, we can give you recommended macronutrient ranges tailored to your goal (e.g. stabilising blood sugars, fat loss, muscle gain etc.).
The Nutrient Optimiser will help you titrate down your carbohydrate intake to the point that your blood sugars stabilise, and then turn to focus more on nutrient-dense high satiety foods and meals that will help you continue your journey towards diabetes reversal and optimal health.


Thank you Marty. Such solid information and so sensible. Enjoy all your information. Thank you
Thanks so much!!!
Brilliant and cuts a straight path through the dogma and wrongheadedness that pollutes the world of nutrition and the LC communities
Thanks Kevin. That was pretty much the goal!
This really helped me understand your statement the other day about keto and fat loss as it relates to blood glucose. Thanks for taking the time to explain!
Cheers. Thanks for reading!
A low fat diet can work as well but I would say that’s probably for a relative minority of people (saturated fat makes me feel like crap) provided the carbs are whole food carbs. I’ve taken my hba1c down from 5.3 to 4.7 using this approach. My fasting insulin was 5 and now it’s 4. That was after 6 months. I haven’t tested it recently. I’ve increased protein and wonder if that will make things take a turn for the worse…
Just the info I was looking for. Very well written and informative!
Thanks for all the time and effort put into these articles here on your website!
Pleasure. Hope it helps.