Jessie Inchauspe, known as the Glucose Goddess, has stormed the wellness arena with her Glucose Revolution.
But how legit is the Glucose Goddess’ approach towards insulin resistance? This review delves into the core of the Glucose Revolution, offering balanced scrutiny to help you discern the hype from the reality. Is it the key to unlocking better blood glucose control?
Journey with us as we unveil what truly lies behind the Glucose Goddess’ methods and the real-world impact they hold for individuals grappling with glucose management.
Free Data Driven Fasting Guide – Improve blood sugar in 30 days
- The Good
- Clothing Your Carbs
- The Not So Good
- What Would I Know?
- More Data Is Not Always Better
- Why Are Glucose Spikes Dangerous?
- The Immediate Problem with Glucose Spikes
- The Dangers of Stable Blood Sugars
- Stable Blood Sugars Do Not Equal Fat Loss
- It’s Your Blood Sugars BEFORE Meals That Matter!
- Do Carbs Turn to Fat?
- Does Insulin Make You Fat, or Is Your Insulin High Because You’re Fat?
- What Does Insulin Do?
- Is Adding Fat to Your Carbs Smart?
- Are ‘Naked Carbs’ Really the Problem?
- Fat+Carb = Hyperpalatable Junk Food!
- Fat and Carbs Raise Your Insulin Levels for a Long Time
- Are You a Unique Snowflake?
- What Causes Your Glucose Rise to More or Less?
- What Raises Your Glucose and Insulin Over the Short Term?
- What Keeps Your Glucose Elevated Over the Long Term?
- How Can You Use Your Glucose to Guide WHAT and WHEN You Eat?
- The Bottom Line
The Good
Jessie Inchauspe is passionate, engaging and immensely likeable.
It’s no wonder she’s built such a massive following on Instagram!
It’s exciting that she’s inspiring so many people to use their blood glucose as an instantaneous window into their metabolic health.
Your blood sugars can be a powerful tool to help you make better choices about what and when to eat.
I love how Jessie and companies like NutriSense and Levels are educating people on how blood glucose data responds to:
- exercise,
- stress,
- elevated blood sugars,
- sleep, and
- hormonal fluctuations.
Jessie highlights that eating protein and fibre earlier in the day or first at each meal positively affects your blood glucose, satiety, and how much you will eat across the day. These principles are central to our approach as well and have helped many people reach their goals in our Macros Masterclass and Data-Driven Fasting Challenges.
Clothing Your Carbs
One of Jessie’s key pieces of advice is to ‘clothe your carbs’ with either protein, fibre, or fat to blunt the glucose response.
As we’ll see later, clothing your carbs might not be such a great idea if your goal is weight loss or to improve your metabolic health. However, there are many benefits that come from adding protein or fibre to your carbs that we’ve detailed below.
Clothing Your Carbs with Protein
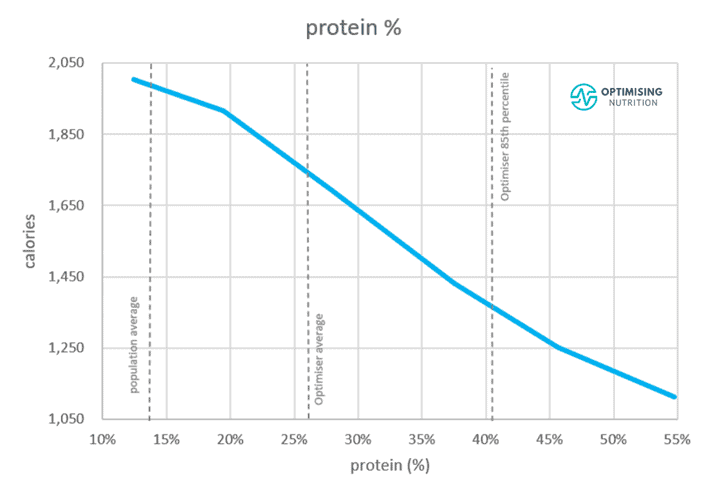
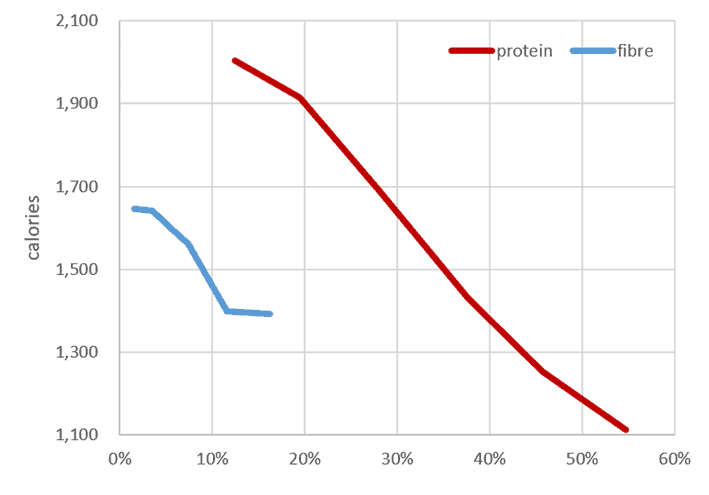
Our satiety analysis of 125,761 days of data from 34,519 Nutrient Optimiser users shows that swapping out some of your non-fibre carbohydrates for protein is the most powerful thing you can do to feel full with fewer calories.
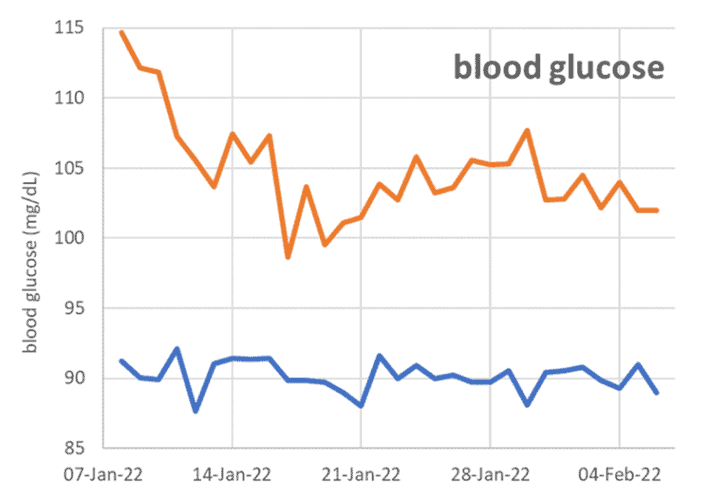
Generally speaking, protein impacts blood sugars minimally. Many people even see their blood glucose drop after consuming a high-protein meal, especially if it’s consumed earlier in the day when their sugars are elevated due to the Dawn Phenomenon. In our Macros Masterclass, we see that it only takes a week or so for elevated glucose levels to fall as people learn to prioritise protein. Meanwhile, people with excellent glucose levels continue to maintain great glucose levels as they shed unwanted pounds.
Because of the power of protein leverage, moving from a low-protein diet to a very high-protein diet corresponds to a massive 55% reduction in calories across the day!
Clothing your Carbs with Fibre
Our satiety analysis also shows that fibre affects satiety positively. However, it’s to a lesser extent than protein. Moving from a low-fibre diet to a higher-fibre diet reduces your overall calorie intake by 16%, or about one-sixth as much as protein.
Our analysis also indicates that moving from refined carbs to minimally processed carbs containing more fibre positively affects satiety, or how full you feel and how much you eat across the day.
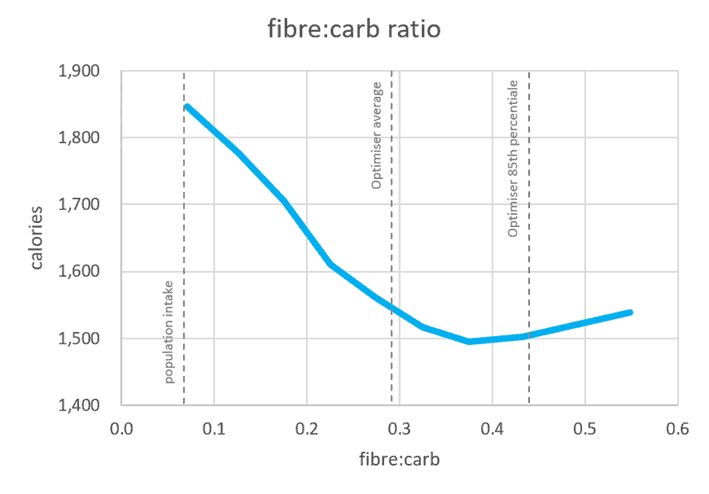
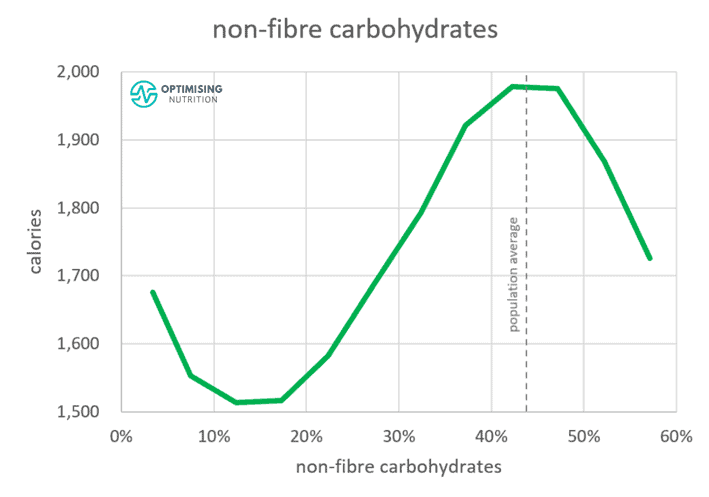
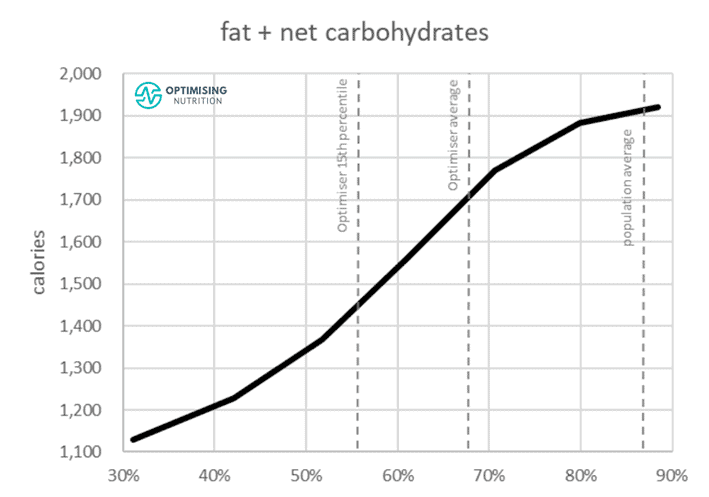
As shown in the chart below, people consuming 40% of their carbs as fibre and maintaining a fibre:carb ratio of 0.4 tend to consume 22% fewer calories across the day.
Minimally processed carbohydrate sources like vegetables or whole grains that naturally contain more fibre are always better choices than refined grains and sugars. Because of their fibre content, they are more filling, and your body takes longer to break them down and does not access the energy they provide so easily. As a result, you are more likely to feel fuller, eat less, and see your blood sugars fall while losing weight without as much conscious control or restriction.
The Not So Good
Jessee makes some good points. However, I am concerned that overanalysing blood sugar fluctuations and a hyper-focus on keeping blood sugars stable will lead people away from their goals of weight loss and improved metabolic health.
As you will see below, some of the common “hacks” that people use to stabilise blood sugars (e.g., clothing carbs with fat) allow us to consume more food. But before long, this leads to increased insulin and higher average blood sugars across the day.
More data can often lead to confusion and overwhelm. If misinterpreted, more data can make us more confidently wrong!
In our Data-Driven Fasting Challenges, we often find that people using CGMs get confused and overwhelmed and give up before achieving significant results. They live in fear of every minor blip on their CGM and throw in the towel when their first 14-day sensor ends.
CGMs often create a state of unsustainable high alert and many questions like:
- why does my morning coffee raise my glucose, and is that bad?,
- will the increase in blood sugar after my workout raise my insulin and make me fat? or
- why does my glucose go low in the middle of the night?
Note: Night-time lows usually occur when people roll over and sleep on their CGM sensor through the night (Freestyle Libre sensors are typically inserted into the shoulder). This limits the flow of interstitial fluid around the sensor and we can see inaccurate and low blood glucose readings, similar to the example shown from my son’s sensor last week. This is known as a ‘compression low’ or a ‘pressure low’, which causes annoying alarms to sound and disturbs sleep.
If you’re one of those people that’s constantly confused by the seemingly infinite array of things that can affect the short-term fluctuations on your CGM sensor, this article will hopefully help clarify what you should focus on to make the most of your blood glucose data.
What Would I Know?
As an engineer who’s married to someone with Type-1 Diabetes, I became fascinated with the myriad of things that affects blood sugars and insulin for the last 20 years as we’ve worked to gain better control of her condition.
In December 2021, my 17-year-old son was also diagnosed with Type-1 Diabetes. Now, I get to watch two CGM traces on my phone and computer pretty much every waking moment.

I have the fascinating privilege of seeing their insulin and blood glucose response to what they eat, their stress, and their exercise. I’ve even charted my wife’s monthly insulin variations to understand how we can tweak her basal insulin rates based on her monthly cycle.
For more detail, see What to Eat for Each Phase of Your Monthly Menstrual Cycle.
Over the past 18 months, we’ve also run fourteen rounds of the Data-Driven Fasting Challenge (DDF). We’ve guided thousands of people through using their blood sugar data to optimise their food choices for better blood sugar control and weight loss.
Our DDF data has also allowed me to field a never-ending array of questions and develop a comprehensive suite of answers to the FAQs.
More Data Is Not Always Better
While data analysis can offer some powerful insights, we’ve found that more data and analysis isn’t always better when it comes to retraining your habits and survival instincts around food. Most people see the best results and make better decisions with the minimum effective dose of actionable data.
Once you learn to recalibrate and train your hunger using your glucose meter as a fuel gauge and eat only when you feel hungry and have validated that you need to refuel, you’re well on your way to taming your hunger monster.
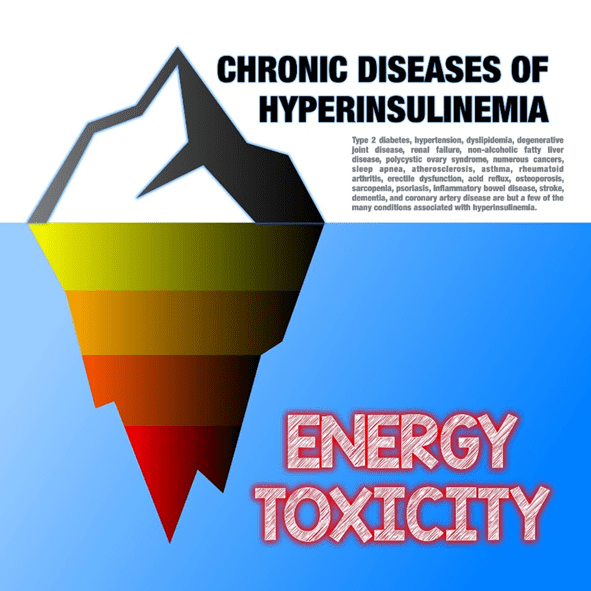
Instead of managing symptoms (blood sugar fluctuations), you’ve addressed the root cause of your metabolic dysfunction (energy toxicity).
My goal here is not to be a critical smart arse. Instead, I hope that this information will help you avoid misinformation that can cause weight gain and worsening metabolic health.
For more info, see Hunger Training… How to Use Your Glucometer as a Fuel Gauge to Train Your Appetite For Sustainable Weight Loss.
Why Are Glucose Spikes Dangerous?
Jessie does a great job of showing that extreme glucose spikes are a problem that many people experience without knowing. While not clinically diagnosed with diabetes, many people are already aboard the blood sugar rollercoaster.
In the science section of her website, Jessie says,
‘When we spike, our mitochondria become overwhelmed and produce free radicals. Free radicals harm our cells, mutate our DNA, and lead to oxidative stress and inflammation.’
Learning to manage your blood sugars effectively can prevent mild insulin resistance from snowballing into prediabetes and full-blown Type-2 Diabetes. The table below shows commonly accepted ranges for healthy blood sugars. If you eat carbs and your blood sugars are in the “normal” range, there’s probably no need to be too concerned.
In our Data-Driven Fasting Challenges, we use slightly tighter ranges and encourage people to dial back refined carbohydrates if their blood glucose rises by more than 30 mg/dL (1.6 mmol/L) after they eat.
If your glucose spikes above this threshold, it simply means that you’ve overfilled your glucose fuel tank with more carbs than you needed.
Tracking blood sugars is a great way to understand which foods are overfilling your glucose fuel tank.
But, as we’ll discuss later, it’s not simply that carbs are bad and fat is good.
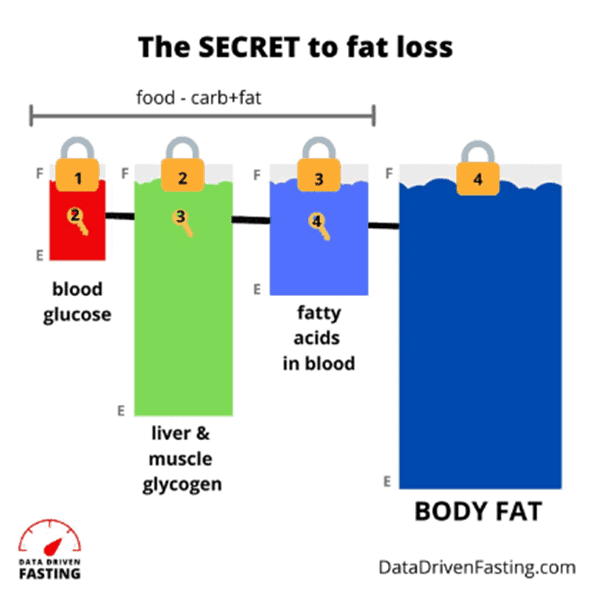
The reason your glucose fuel tank is overflowing is most likely because your fat stores are also full.
The Immediate Problem with Glucose Spikes
While there is a long list of complications linked to elevated blood sugar levels, the immediate problem with glucose spikes is the crash that often follows.
When you eat excessive amounts of refined carbohydrates, your pancreas will increase your insulin levels to stop the release of your stored energy into your bloodstream so it can use the glucose from the food you just ate.
But, as they say, what goes up must come down! When your blood sugar comes crashing down, hunger will kick in, and you will search for food to bring your levels up and give your brain the glucose it needs.
There’s no negotiating with your inner hunger monster when your blood sugars have dropped way below what is normal for you. The further your blood sugar falls, the more likely you will make poorer food choices and overeat hyper-palatable fat-and-carb combo foods.
Once you give in to your overwhelmingly intense hunger and inevitably gorge on less-than-optimal foods, your blood sugars skyrocket back up, and the process repeats.
This ‘blood glucose rollercoaster’ leaves many people feeling as if they are ‘addicted to food’.
Reducing your carbs to achieve healthy blood glucose variability is a critical first step towards managing your appetite and hunger to allow you to make better food choices.
Interestingly, most people in our challenges find that they don’t need to reduce their carb intake significantly. Instead, many people–especially those from a low-carb or keto background—see firsthand that whole-food carbs are nothing to fear as they leave their blood sugars in a healthy range, especially if they’re consuming a nutrient-dense diet with adequate protein.
As we will discuss later, many people who previously lived in fear of carbs learn to strategically use carbs to quickly quench their appetite when their blood sugar is below normal for them. This brings their blood sugars back up into the healthy range without resorting to energy-dense, nutrient-poor comfort foods that we typically reach for when we’re starving!
The Dangers of Stable Blood Sugars
One of the problems with chasing stable blood sugars as your primary goal is that people often swing to the other extreme.
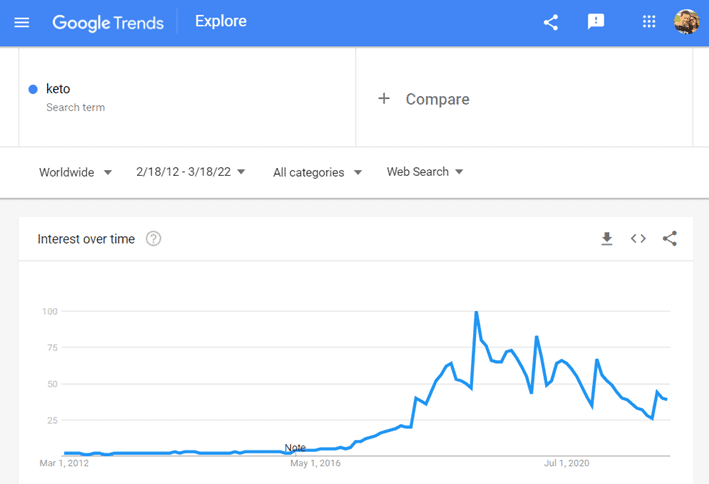
Because high-fat foods tend to increase blood sugars the least over the short term, many people replace carbs, and even protein, with refined fat. This line of thinking was all the rage during the keto heydays.
I remember talking to a doctor wearing a continuous glucose monitor at a Low Carb Down Under conference when they were first available. He told me he was eating minimal protein and carbs and ‘fat to satiety’ to stabilise his blood sugars, his insulin would stay low, and he would lose weight. But looking at him, it sadly didn’t look like it was working well for him. He looked puffy and inflamed.
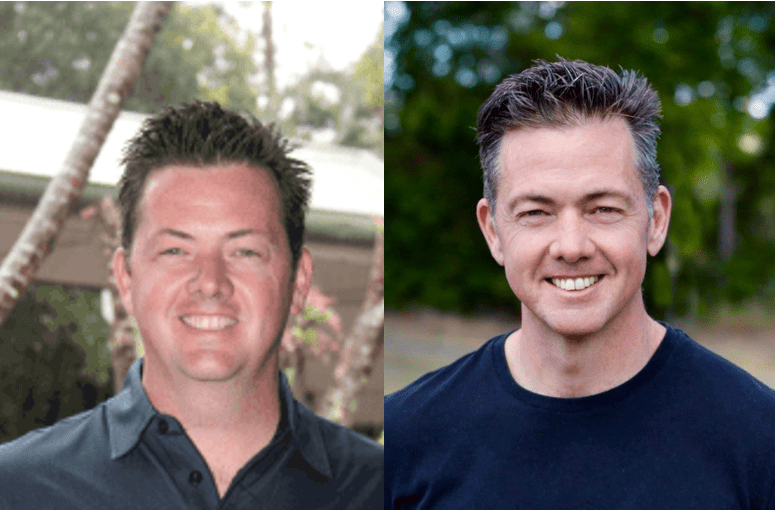
Like this doctor, I once chased higher ketones by upping my dietary fat intake when I got on the keto bandwagon. At the time, I believed I would lose body fat because my insulin levels would be low. I thought my metabolism would behave like a person with uncontrolled Type 1 Diabetes who couldn’t produce enough insulin.
My keto phase didn’t work too well for me either, and I gained more weight! The photo on the left is me during my ‘just keto harder’ phase. Eventually, I realised that fat is not a free food and I could not simply ‘eat fat to satiety’.
Note: Jessie even mentions gaining weight on high-fat keto when trying to flatline her blood glucose in her book and one of her videos.
Stable Blood Sugars Do Not Equal Fat Loss
While many people believe that stable blood sugars equate to fat loss, it’s not that simple.
While lean and metabolically healthy people tend to have stable blood sugars and tolerate carbs well without seeing a sharp rise in their blood sugar, simply managing the symptoms by manipulating your diet to achieve stable blood sugars will not make you lean and metabolically healthy.
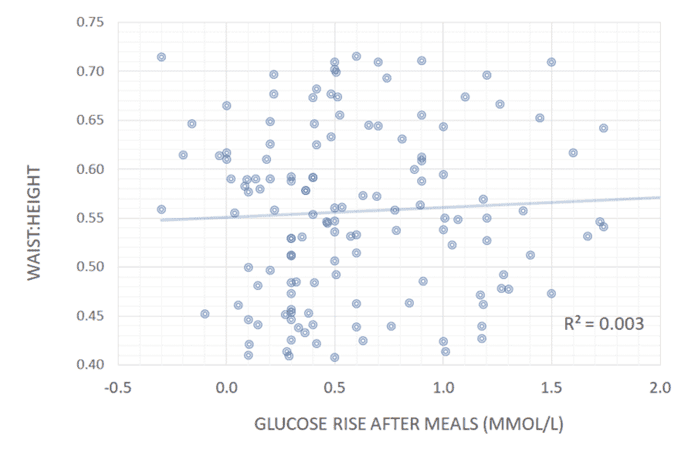
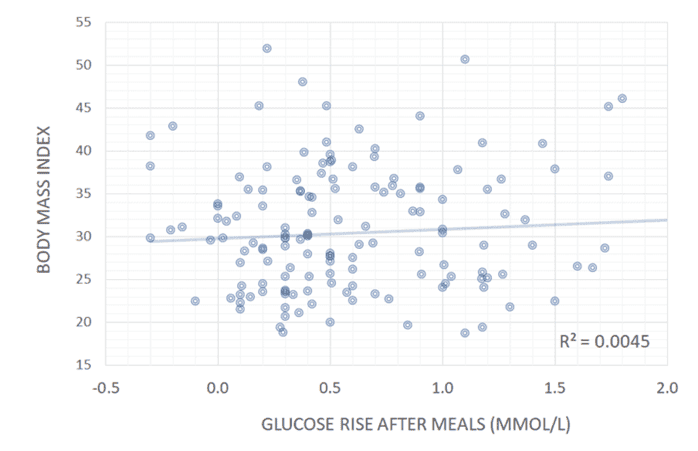
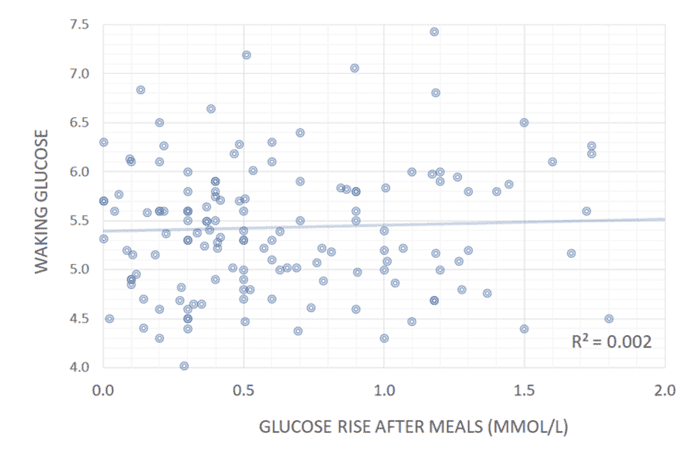
The chart below shows data taken from our analysis of people doing our Data-Driven Fasting Challenges. We see no correlation between stable blood glucose readings and waist-to-height ratio, body mass index, or waking glucose levels.
While lean and metabolically healthy people have stable blood sugars–like Jessie’s boyfriend, who can eat cookies without his glucose spiking–managing the symptom (glucose spikes) by adding fat to your carbs does not improve blood sugars.
As you will see, eating ‘fat to satiety’ and avoiding all carbs and even protein will likely make matters worse. But ‘clothing your carbs’ by adding fat to ‘blunt the blood sugar response’ is perhaps the worst thing you can do for your metabolic health, average blood sugars and HbA1c.
For more details, see:
- How to Use a Continuous Glucose Monitor for Weight Loss (and Why your CGM Could Be Making You Fat),
- Keto Lie #5: Fat is a ‘Free Food’ because it Doesn’t Elicit an Insulin Response
- Keto Lie #11: You Should ‘Eat Fat to Satiety’ to Lose Body Fat
It’s Your Blood Sugars BEFORE Meals That Matter!
The chart below shows our analysis of participants in our Data-Driven Fasting Challenges. We can see that your PRE-meal blood sugars align with healthier waking glucose, weight, and metabolic health.
If you want to lose weight and improve your metabolic health, you need to adjust WHAT and WHEN you eat so your blood sugars fall just a little below what is normal for you.
At this point, you will be using less glucose and more of your stored body fat for fuel. You will also experience true hunger, but without being so ravenous that you will eat anything and everything you can to survive!
While there are plenty of ‘hacks’ you can use to manipulate your blood glucose rise after a meal, there are no simple hacks to lower your premeal blood glucose that don’t also align with improved metabolic health and your actual need for more food.
For more details, see How to Use a Continuous Glucose Monitor for Weight Loss (and Why Your CGM Could be Making You Fat).
Do Carbs Turn to Fat?
On her science page, Jessie says,
‘When we spike, insulin is released, and excess glucose is stored as fat.’
This is partially true, but it is also largely irrelevant.
We CAN convert glucose to fat via de novo lipogenesis, the process where your body synthesises fat for storage from glucose. However, due to oxidative priority, your body will prioritise using the energy from the carbs you eat, and fat will go to the back of the line. Hence, glucose is ‘fat-sparing’ most of the time.
The only situation where de novo lipogenesis from carbs would be significant is if you consumed a LOT of carbohydrates with very little fat. As we’ll see later, this is hard to do.
See Oxidative Priority: The Key to Unlocking Your Body Fat Stores for more details.
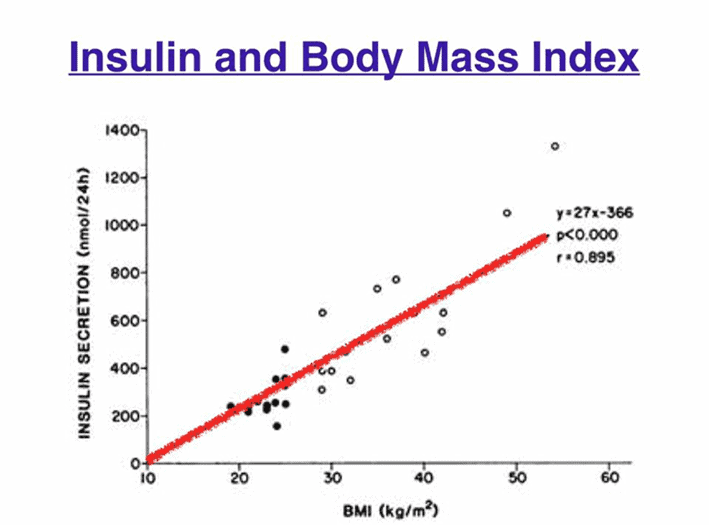
Does Insulin Make You Fat, or Is Your Insulin High Because You’re Fat?
‘Weight loss is always preceded by insulin levels lowering. Therefore, lowering insulin is key to weight loss.’
This is perhaps the most significant misinformation still endemic in the keto movement. Unfortunately, I fear it will live on beyond the death of keto because so many people are now hyper-fixated on their CGMs in the hope of stabilising their blood sugars and insulin with the mistaken belief that it leads to fat loss.
While we often hear about the anabolic role of insulin–to make things bigger and help store energy in our body–it’s critical to understand that the primary role of insulin is anticatabolic: that is, to stop your body from breaking down and disintegrating.
More than 80% of the insulin my wife and son require each day as Type-1 Diabetics is unrelated to the food they eat; it’s required to prevent their stored energy (as fat, muscle and organ tissue) from flooding into their bloodstream.
This is no different for the 98.5% of us with a fully functioning pancreas. The more energy you have stored in your body, the more insulin you need to store it. Trying to manage your insulin levels by measuring the blips on your CGM is like measuring the ocean’s volume by measuring the waves’ height at the beach on a calm day. If you focus on the wrong metric, you become more confidently wrong!
What Does Insulin Do?
If you accidentally inject too much exogenous insulin, your liver will slow the release of glucose and fat into your bloodstream. As a result, your blood sugars would drop, your hunger would engage, and you’d be driven to overeat.
But, if you are part of the fortunate 98.5% of the population who have a fully functioning pancreas and NOT injecting exogenous insulin, this “fun fact” is entirely irrelevant for you.
Your body is highly efficient. Thus, it won’t make more insulin than it requires to keep your stored energy locked away while you continue shovelling low-satiety, nutrient-poor, hyper-palatable ‘food’ into your mouth!
When you learn to eat in a way that increases satiety, you will consume less energy, so your pancreas will lower insulin to allow more of your stored energy into circulation to be used for fuel. Later, once you achieve a lower weight, your insulin levels across the day will be lower because you have less fat to hold in storage!
Yes, insulin and obesity are correlated. But unless you’re injecting insulin, high insulin levels are the result of obesity, not the other way around!
- It’s not weight loss -> decrease insulin levels, but rather
- weight gain -> increase your insulin levels.
Understanding the direction of causality is critical! The most effective way to reduce your insulin is to increase your satiety. This will allow you to lose weight with less hunger and hence your body will need to produce less insulin.
For more details, see:
- What Does Insulin Do in Your Body?,
- Personal Fat Threshold Model of Insulin Resistance, Diabetes and Obesity, and
- How to Reverse your Insulin Resistance
Is Adding Fat to Your Carbs Smart?
Next, we come to Jessie’s most concerning recommendation of “clothing your carbs with fat”.
The snip below is from an interview with Jesse in the Daily Mail promoting her book, Glucose Revolution. In it, she recommends putting ‘clothes on your carbs’ and ‘always eat your bread with butter’.
To be fair, the focus on her recommendation to ‘add butter to your carbs’ may be Jessie’s publicity team or the Daily Mail picking out what they think people want to hear will help them lose weight and improve their diabetes. Whether this is the case or not, I think it’s worth highlighting how counterproductive this could be!
‘Clothing your carbs’ with protein and fibre is a sound recommendation, but adding fat to your carbs to simply manage the annoying squiggly line you see on your CGM trace is bad advice! In fact, adding fat to your carbs is the most effective and efficient way to fatten up!
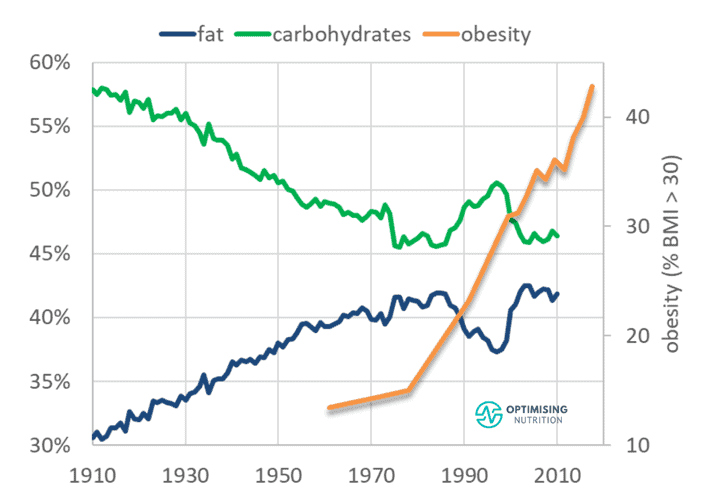
Carbs aren’t any more fattening than dietary fat, and vice versa. Your body does fine with one or the other. But we get into trouble when we combine them in similar amounts in ways that we don’t find in nature!
Foods like nuts and milk that combine fat and carbs are rare in nature. Generally, they’re only available at particular times of the year or for a specific purpose, like in autumn for animals to fatten up or so babies can grow. These foods stimulate our dopamine system times two, incentivising us to eat more. During more primitive times, when we evolved, this would help guarantee our survival.
Today, modern processed foods are formulated to combine processed industrial seed oils and refined grains to increase their palatability. Unfortunately, as more of our processed foods have implemented this tasty and fattening formula, the obesity epidemic has spiralled upwards!
Are ‘Naked Carbs’ Really the Problem?
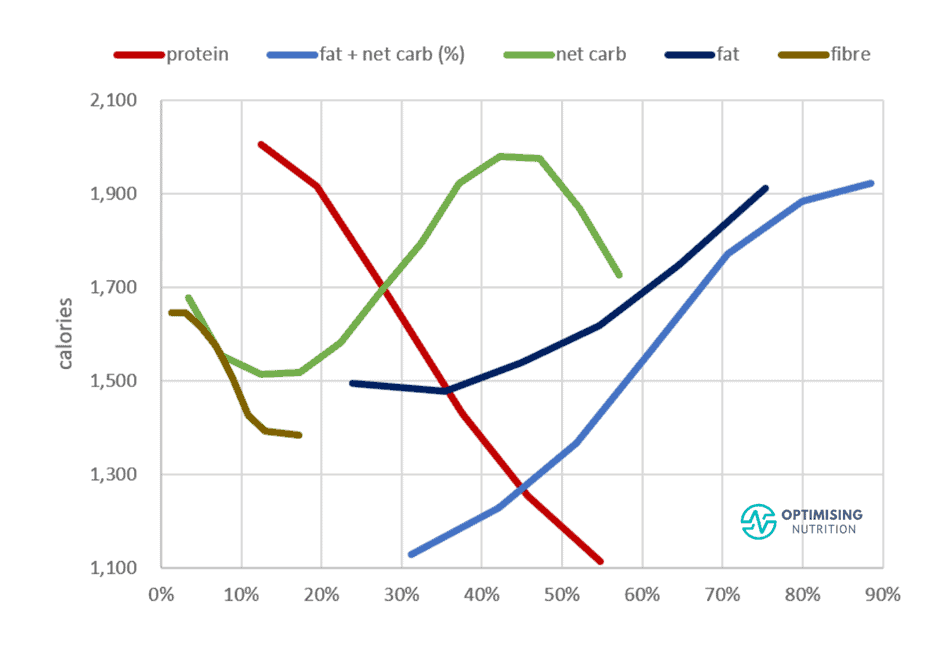
The chart below shows our average satiety response to non-fibre carbohydrates.
To the left, we see we tend to eat the least when 10-20% of our calories come from carbohydrates.
However, to the right, we see that our calorie intake also decreases if we’re eating a very high-carb (i.e., more than 50% carbs) low-fat diet if we move to the right.
Our data suggests that very few people tend to stick to a low-fat, high-carb diet. However, it wouldn’t make you fat if you did.
It’s hard to get fat from eating too much plain rice or too many potatoes, tomatoes, and broccoli. In fact, there are small communities of very lean people living on unprocessed, low-fat, plant-based foods.
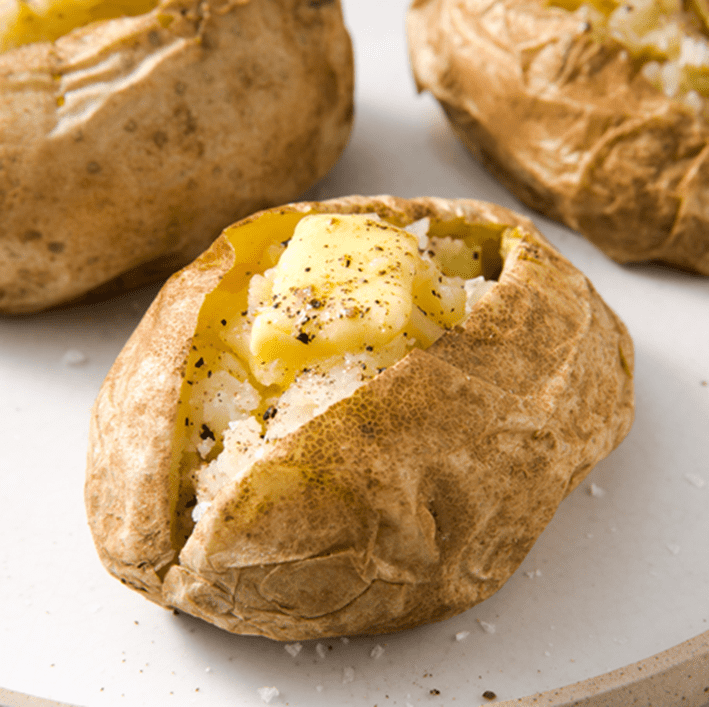
There is even a ‘Potato Hack Diet’ that works because of how impossible it is to overeat plain (unbuttered) potatoes.
But when we add fats like butter and oil to the seemingly harmless potato, we get crisps that are easy to overeat because they give us a massive hit of dopamine that tells us to EAT MORE NOW!
When we add butter to our spuds, we’re effectively giving them the same nutritional profile as a cheesecake, doughnut, or piece of pizza! This combo fills our glucose and fat fuel tanks simultaneously, and all of these foods are similarly high in carbs and fat and low in protein.
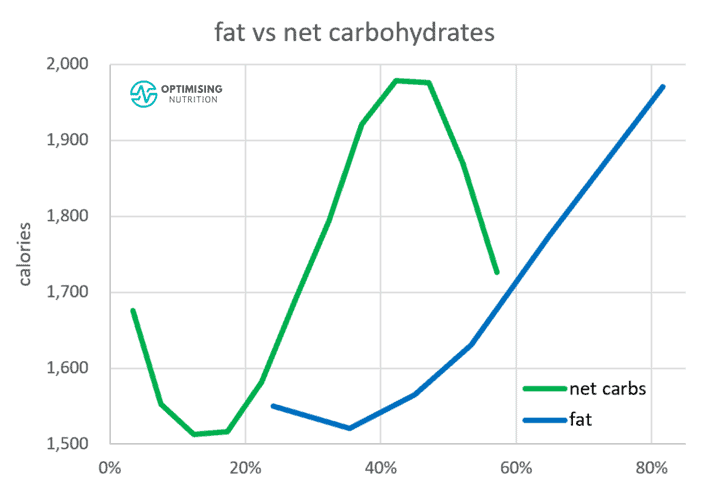
It’s interesting to note that our satiety response is similar when we reduce either fat or carbs. Reducing your net carbs from 45 to 15% or your fat from 80 to 40% are both effective ways to help you eat less by similar amounts of calories.
Have you ever wondered why we see the ongoing wars between the low carb vs the low-fat factions? It’s because both of them work!
Sadly, while the low-fat vs low-carb war rages on, most people are left confused in the middle, chowing down on foods that are a similar blend of fat and carbs, confused as to why their weight and blood sugars and waistline are climbing.
For the uneducated consumer, these foods taste SO good, and we can overeat them easily. The chart below shows our satiety response to the hyper-palatable fat and non-fibre carbohydrate combo. As we continue to ‘clothe our carbs’ more by adding more fat to them, we eat more. As shown by the line on the far right-hand side, the majority of the population is consuming the perfectly fattening combination of fat and non-fibre carbs!
Conversely, you can gradually reduce your carbs or fat–or ideally, both–while still prioritising dietary protein and fibre so you can eat less without feeling hungry. This is the process that we guide people through in our Macros Masterclass.
The chart below shows the satiety response of all of the macronutrients combined in the same chart. The biggest impact comes from progressively reducing fat and (or) carbs which leads to a higher protein %.
For more details on how we walk people through managing their blood sugars in the Macros Masterclass, see FAQ #3.
Fat+Carb = Hyperpalatable Junk Food!
Many people would see the foods in the photo below as ‘bad carbs’.
The reality is that these foods are ’bad’ because they are a similar combination of fat and carbs together with minimal protein and fibre. While they will keep your blood glucose levels relatively stable, they will also keep your blood sugars from falling below your baseline for many hours and even days!
The best way to improve your blood sugars and reduce your waistline is to not to aim for stable blood sugars but rather to simply wait to eat until your glucose is a little lower than normal for you.
As you chase a lower premeal trigger and the glucose in your body is depleted, your body turns to your unwanted, stored body fat for fuel.
Fat and Carbs Raise Your Insulin Levels for a Long Time
I have the privilege of watching my wife Monica’s CGM and closed-loop insulin pump system every waking hour.
The screenshot below shows her blood glucose and the basal insulin that her closed-loop pump system is constantly adjusting to keep her blood sugars in a normal healthy range. The blue chart in the middle is her basal insulin rate on her pump, which continually adjusts in response to the changes in her blood sugar levels.
While she tries to avoid it, her blood sugar doesn’t ‘spike’ like you’d expect when she eats foods like pasta carbonara at a restaurant when the pickings are slim. Instead, her glucose rises but stays elevated for up to 36 hours from a single meal! I also see the closed-loop insulin pump algorithm hammering away and pumping out more and more insulin to try and bring her glucose levels down.
For decades, people with diabetes have been advised to eat some fat with their carbs to reduce their postprandial spike. However, this is sadly the worst advice you could follow to lose weight, lower your insulin levels, and control or prevent a metabolic condition!
‘Clothing your carbs’ with protein and fibre is excellent advice. However, dressing your carbs with extra fat is the most effective way to eat more, increase your long-term insulin and the area under your blood glucose curve, and–before long–get fatter.
Are You a Unique Snowflake?
Another thing that frustrates me is the explosion of people using CGMs to find their ‘unique’ biochemical response to food. People watch their CGM endlessly like a fortune-teller gazing into their murky crystal ball, looking for the ‘secret’ to unlocking their own ‘unique’ metabolism.
But it’s not that complex!
While we’re all slightly different, you’re likely NOT a unique snowflake.
Your blood sugar rises more in response to different foods for straightforward reasons.
Hint: It’s not your microbiome, and you don’t have to send your ‘poo in the post’ in for analysis to understand why your glucose rises more than your friend’s.
The simple primary factors that influence your blood sugar and insulin after eating are:
- the macronutrient profile of what you ate, and
- how fat you are!
What Causes Your Glucose Rise to More or Less?
The biggest reason your glucose rises more or less than your friend’s after eating the same food is that you have more or less energy stored in your system as fat and glucose.
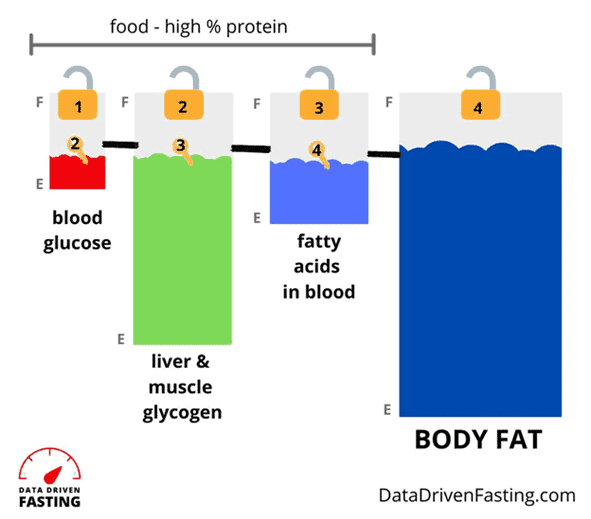
The glucose and fat fuel tanks in your body are separate but interconnected. Because you have limited room to store glucose, it must be used first.
If your body fat capacity is full or overflowing, all the fuels will back up in your system, and any dietary glucose will quickly show up on your CGM trace. Your glucose tanks are full, but your fat tanks are also full, leaving the stored fuel in your body to back up in your system.
As you dial back the energy in your food from both fat and non-fibre carbs and begin prioritising foods and meals with more nutrients, fibre, and protein, you will deplete your glucose and fat fuel tanks, including your overfull body fat (adipose tissue) fuel tank.
Now, when you eat carbs, your body can easily store and utilise that energy, and you won’t see such a large spike on your CGM!
For more details, see Oxidative Priority: The Key to Unlocking Your Body Fat Stores.
What Raises Your Glucose and Insulin Over the Short Term?
The Food Insulin Index data helps us predict how foods will affect our blood sugar and insulin levels in the three hours or so after we eat. In summary:
- Glucose raises blood sugars and insulin the most over the short term. However, they also return to baseline quickly if it’s eaten without added fat.
- The fructose in your food has a much smaller impact on your blood sugar and insulin than carbohydrates because it is converted to fat in the liver.
- Fibre has a negligible impact on insulin and glucose because we do not have the enzymes to break it into usable energy.
- Protein requires about half as much insulin as carbs in the first three hours after it is consumed. But beyond these three hours and over the longer term, protein increases satiety and thus decreases your insulin across the day.
- Fat impacts glucose and insulin levels minimally over the short term. But because it is so low on the totem pole of oxidative priority, it is stored easily. If you continue consuming more fat than you use over the long term, you will end up needing more basal insulin because of your increasing body fat levels.
For more info, see:
- Making Sense of the Food Insulin Index, and
- What Foods Raise Your Blood Sugar and Insulin Levels After Eating (Other Than Carbs)?
What Keeps Your Glucose Elevated Over the Long Term?
The problem with the Food Insulin Index data is that it only considers our response to food over the first three hours. If you only used this to guide your food choices, you would avoid carbs and even protein and just consume fat.
However, the reality is that dietary fat elicits an insulin response over the long term. Because there is plenty of room to store fat on your body, your pancreas doesn’t raise insulin levels as it does with carbs to ensure they are used before more stored energy can be released. Dietary fat is welcomed aboard to be used later as a result.
While dietary fat doesn’t raise your CGM trace abruptly, it prevents your blood sugar from falling for longer. So, the more fat you eat, the longer you will have to wait before your body needs to tap into the fat stored on your body again.
As depicted in the chart below, good blood sugar management is about reducing the area under the curve of your insulin and glucose responses after eating.
- Carbs will raise your blood sugar and insulin quickly.
- Dietary fat will keep your blood sugars and insulin elevated for longer.
To get your blood sugars down sooner, you need to reduce the energy from both fat and carbs in your diet while still prioritising nutrients and protein.
How Can You Use Your Glucose to Guide WHAT and WHEN You Eat?
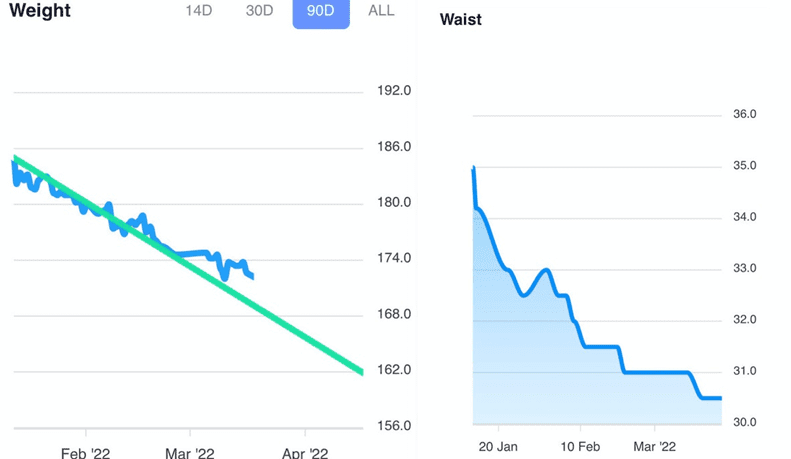
Before we wrap up this ‘review’, I want to show you how we use your blood glucose to guide WHEN and what you eat in the Data-Driven Fasting Challenges.
Many people in our challenges use a continuous glucose monitor. However, if they don’t already have one or can’t afford a CGM, an accurate glucometer is fine.
Chasing Your Premeal Glucose Trigger
This first chart shows how someone chases their premeal glucose trigger.
After three days of baselining, they get their premeal blood glucose trigger, which is simply the average of their glucose just before they eat over three days.
From there, they simply wait until they are hungry, and their glucose indicates that they need to refuel to eat.
As you continue to do this successfully, your premeal blood glucose trigger decreases in the Data-Driven Fasting app.
Reducing Glucose Spikes
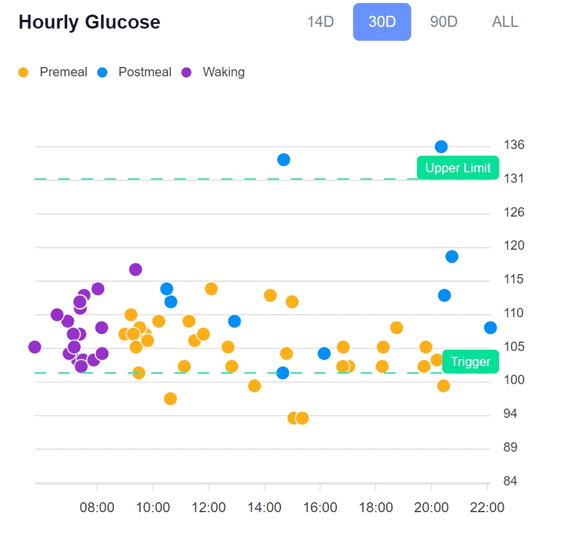
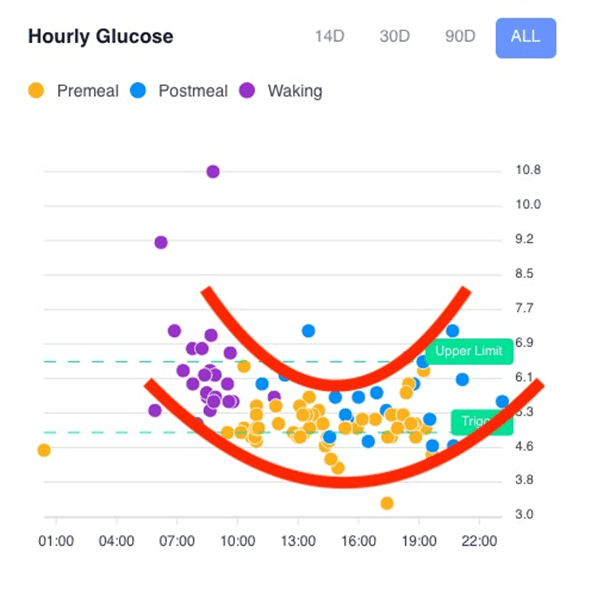
The figure below shows the long-term (90 days) and short-term (14 days) hourly glucose charts in the DDF app from one of our participants, Christina.
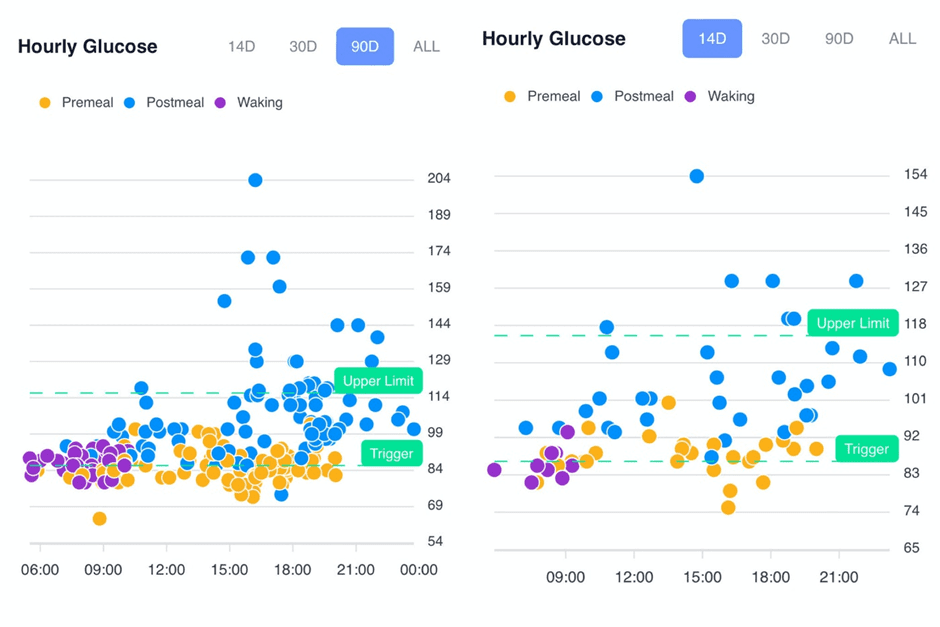
In the first chart, you can see that there are a lot of data points above her upper limit (i.e., more than 30 mg/dL above her current glucose trigger). Over time, she has learned to reduce the number of times she overfills her glucose fuel tank by making more intelligent food choices that don’t spike her blood glucose levels.
As she has chased a lower trigger and prioritised nutrient-dense foods, she has also drained her body fat stores. This has allowed her to tolerate more carbs without seeing significant glucose spikes.
Using your Glucose to Guide WHAT to Eat
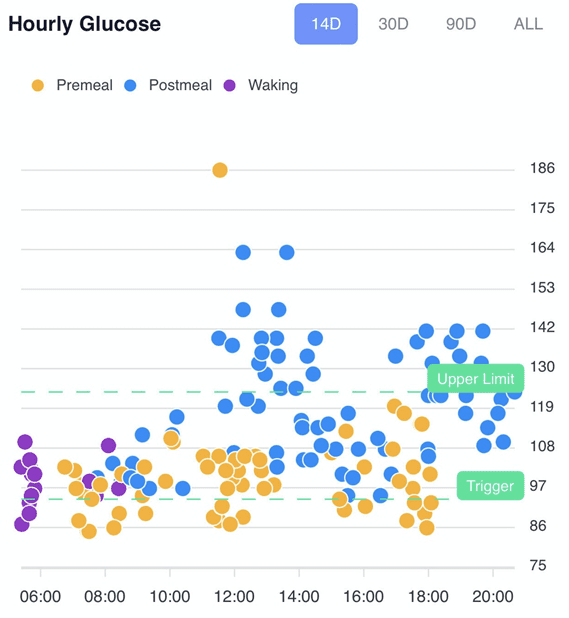
But where this gets even cooler is when we see we can use our glucose trends to guide what to eat across the day. It’s fascinating to see how everyone has a slightly different pattern in their blood sugars!
In the example pattern shown below, we see slightly higher blood sugars in the morning due to dawn phenomenon. Slightly higher glucose levels earlier in the day is a typical pattern that we see in lower-carb dieters, whereas people following a lower-fat diet tend to see the reverse.
If your blood sugar is higher and above your trigger in the morning, it’s a good time to prioritise protein, which usually comes with some fat. Protein earlier in the day keeps people full, and many people see their blood sugars fall rather than rise a few hours later. This means they’re good to eat again sooner if they are hungry. But if you know from your glucose meter that you already have plenty of fuel in your bloodstream, all you need is nutrients and protein, with less energy from fat or carbs.
Prioritising meals with more carbs and less fat later in the day or after exercise may be more appropriate to raise blood sugars without falling into the hyperpalatable fat and carb danger zone if your blood sugars are below your trigger.
Prioritising carbs with less fat will enable you to satisfy your hunger quickly without reaching for the energy-dense carb-and-fat combo comfort foods that we all tend to overeat when we’re hungry.
Meanwhile, other people find they have lower blood sugars in the morning and do better with more carbs with their protein at their first meal and fewer carbs later when their body doesn’t appear to tolerate them.
Others start to see a pattern indicating that they need to eat their biggest meal when their blood sugars are lower in the early afternoon. Your blood sugars can offer fascinating and powerful insights about WHEN and WHAT to eat!
The Bottom Line
- Your blood sugars can provide powerful insights to guide WHAT and WHEN you eat.
- Simply eating to stabilise your CGM trace can lead people to consume foods and meals that worsen their metabolic health.
- Fat and carbs are both energy sources for your body. Consuming carbs with protein and fibre will help improve satiety and minimise the blood sugar response.
- Adding fat to your carbs will lead you to overconsume these foods and see larger insulin and blood glucose responses over the long term.
- Your blood sugars before you eat are the most powerful indicators that you can use to guide when you eat.
- You can use your premeal blood glucose as a guide to ensure you are using your stored energy and not adding to it, which would drive insulin resistance and worsen metabolic health.
- You can use your glucose data to make more intelligent choices on WHAT to eat while staying out of the fat-and-carb danger zone.
Data Driven Fasting – Improve blood sugar in 30 days or money back guaranteed.
More
- Blood Glucose Spikes: When to be Worried and How to Prevent Them
- Data-Driven Fasting: How to Lose Weight and Reverse Type 2 Diabetes Without Tracking Your Food
- Hunger Training… How to Use Your Glucometer as a Fuel Gauge to Train Your Appetite For Sustainable Weight Loss
- How to Use a Continuous Glucose Monitor for Weight Loss (and Why Your CGM Could Be Making You Fat)
- What Foods Raise Your Blood Sugar and Insulin Levels After Eating (Other Than Carbs)?
- Oxidative Priority: The Key to Unlocking Your Body Fat Stores





















This book is way too little, way too late–anybody who’s marched to the beat of Jimmy Moore, or you, or several doctors who’ve ended up on Jimmy’s prior podcasts (Eric Westman comes to mind) already KNOWS the little bits of “accurate” info that’s in there, and knew it for YEARS! Someone is clutching at straws trying to wring the last dime out of keto. It’s a shame, because we’ve pretty much all have been there, done that, and have the regained weight to prove that keto pushers love you to get on the program, but nobody ever tells you when to get off it…until you came along. Nobody ever tells you that keto only works once, but your waistline does.
Keto: “But everybody’s doing it–why has it stopped working?”
Carnivore: “It’s working…for now, but I’m constipated, and I’d KILL for a salad!”
P:E: “Ahhh, meat AND salad–but so many egg whites, and so little satiety!”
Vegan: “As long as my food doesn’t have a face, to hell with the macros!”
Pyramid/MyPlate/gastric bypass: “Miss me yet?”
LOL! I fear that the CGM craze will just perpetuate the keto lies and focus people on the wrong goal, and meanwhile, line the pockets of Abbot and Dexcom and drain the health insurance funds that could be better spent on other things like insulin for T1Ds who can’t afford it.
So instead you want people to stab their fingers 20 times a day to find when it’s time to eat? At least the cgm only has to go in once. And how does people paying out of pocket for cgms take away funds for insulin? No insurance or health agency is covering cgms for non-insulin-dependent diabetics
As long as people focus on the right thing, most people do fine on a CGM with DDF. However, focusing on the wrong data can lead to increased confusion. Most people find they end up checking their blood sugar two or three times a day to validate their hunger.
CGM’s are not cheap. My understanding is that companies like Levels and NutriSense write you a script that allows the cost of the CGM to be covered by health insurance/Medicare and then they charge for the nutritional advice and the app. We self fund my wife CGM for her T1D and I can tell you it’s not cheap if you’re paying out of pocket. Diabetes is lucrative for companies like Abbott, Dexcom, NovoNordisk etc.
Great review – courteous and well explained. I especially enjoyed reading the part where you explain what raises your blood sugar more and what keeps it raised longer.
thanks Karen! glad you found it useful.
Wow! Although I found this a little hard to read due to ‘terminology’, I was fascinated nonetheless. This makes sense as to why after a 33kg loss, I have suddenly stalled?. I would love to know more. I’m not interested in weighing my food or calculating “macros” (never have!), but rather I would like to focus on keeping my BGL’s to a “normal” level. I’m a type 2 (in remission) with other medical conditions (also in remission apparently). Thank you for the interesting read.
Thanks Helen! Congrats on your 33 kg weight loss! Lots of people stall out due to adding more fat than they need in the pursuit of the wrong primary goal (e.g. elevated ketones of stable blood sugars). My key point is that it’s your glucose level before you eat that you need to focus on lower if you want to continue to progress by addressing the address the root cause rather than just managing the symptom. As your premeal blood sugars lower, your weight and blood sugars stability will continue to follow.
Thanks so much for this thoughtful and thorough review – extremely helpful! However, as someone who is both, very thin (due to inflammatory etc. issues still working on with various doctors) AND prediabetic for almost 10 years now, I often become confused as to the coupling of metabolic health (what I am after) with weight loss (I need to gain). As a post menopausal woman, I probably carry visceral fat in my abdominal region, so probably want to be losing that for optimal health, yet I also want to gain (muscle? fat?) as well. I wonder if any one in the DDF community has experienced this…
I am looking forward to joining a future DDF challenge (April may not work due to air travel during that time and I’m not keen on pricking my fingers in airports LOL)
Again, thanks so very much for the work you are doing – I have been slowly working my way through Big Fat Keto Lies and finding it very, very informative.
Thanks Jennifer. Some people have a lower personal fat threshold, meaning their adipose tissue can’t store as much energy before backing up into their bloodstream. Gaining muscle and losing fat is all about getting enough protein without excess energy (and ideally with some resistance training thrown in for good measure). DDF will help with blood sugars, but given you’re already thin, our Macros Masterclass may be more useful. https://optimisingnutrition.com/macros-masterclass/
Excellent review Marty, polite and explained in great detail! After hearing of Jessie, recommended by someone here, I followed her for 3 days. Once I saw that she was eating things like chocolate cake and recommending ways to mitigate the glucose rise I stopped wasting my time. I don’t eat those kinds of foods as it’s so much easier to just avoid them completely. Thank you for all you do to intelligently inform on the right way to optimal health!
Thanks Lori! Hopefully, this “review” helps people avoid chasing the wrong goals and going confidently wrong.
Thanks for the article.
(I have T1 and a CGM: I have wondered why anyone without diabetes would go to so much trouble if their life didn’t depend upon it.)
CGMs are awesome for people who need them to live. But we see they tend to cause a LOT of confusion for most people. More data is not always better. A simple glucometer gives all the data you need to verify that you need to refuel. It also avoids the temptation to try to manage the annoying CGM trace with hacks such as adding fat to your carbs believing that it’s going to lead to weight loss and health.
Great post as ever Marty. You are so much ahead of the curve on this one – I’m so glad I read this post today (Jessie’s Audible book is released in the UK today, and I have that on back-order after hearing her on Siim’s podcast). I have incorporated many of your learnings into the work I do with my Nutrition & Lifestyle Clients. I do have a burning question for you though (!) You have mentioned before (as per the graphs above), that your Optimisers spontaneously eat the least calories when their non-fibre carbs are 15%, and their dietary fat is 35%. So, clearly this leaves 50% left… My question therefore is: is this remaining 50% protein only (ie the 100% split is based on total calories) or is it instead 50% protein + fibre (ie 100% split is based on all macros). And if it is the 2nd scenario – any thoughts on how the protein/ fibre is split over the 50%? I’m dying to know!
Thanks Marty for all the great work you do (and of course to Ted’s amazing graphics which always make me smile!)
The macros are independent variables. Max satiety tends to occur with < 40% fat, 10-20% non-fibre carbs and the rest being protein and fibre. But rather than jumping from one extreme to another, we tend to see people do the best when they move from where they are towards "optimal" by dialling back fat and carbs (i.e. clothed carbs).
Thanks for clarifying Marty, if you ever get the data it would be great to know what fibre % is associated with least spontaneous calorie intake, but harder to measure I guess since not so clear cut as counting grams of protein.
In terms of ‘clothed carbs’, I totally agree when it comes to ultra-processed foods which incorporate both fat and carbs which are not found in nature (ice-cream, bread and butter etc). However, I was listening to Maria Emerich recently on a podcast who was dead against consuming even natural foods such as avocado + almonds together because of ‘clothed carbs’. Personally, with my clients I have not found that eating 2 x natural ‘fat + carbs’ foods together is any problem at all – with the key to it being that both the fat (avocado) and carbs (almonds) come bundled with fibre – which crucially is not added/ milled fibre but fibre within the natural food matrix. In my experience, fibre which is held in its natural food matrix ameliorates any issues with natural ‘clothed carbs’. Do you have any data yet to support/ dismiss that?
The fibre that you get from nutrient-dense whole foods is great, but it has only about one-sixth of the impact compared to protein. I have a section here on fibre and the fibre:total carb ratio – https://optimisingnutrition.com/micronutrient-ratios-and-why-they-are-important/#h-fibre-carbohydrate-ratio
Natural fat+carbs combos like nuts, full-fat dairy and avocado can be a great way to maintain weight, but if you want to lose weight, many people find they need to cut back on those foods. Modern processed foods are just the extreme end of that spectrum. See this chart from the article above for details (blue line shows fat+carb combo, the brown line is fibre) – https://optimisingnutrition.com/wp-content/uploads/2022/03/image-199.png
Very interesting Marty – that tells me that ‘ideal’ protein range is somewhere between 39% – 50%, with fibre correspondingly between 0-11%. Many thanks!
Yes. But keep in mind that ‘optimal’ and sustainable are two different things. Sharp and effective tools can be dangerous in the wrong hands. In our Macros Masterclass, we’ve actively tried to calm people down and guide them towards optimal, starting from where they are now. We’re seeing much better long term results, less rebounding and less mental anguish.
great and detailed review. Physiologically, it makes full sense. Underscored by your data and related effects in patients, you are to me the most scientific knowledgeable person on treating diabetes and the underlying mechanisms. keep up the good work.
additional comment: while you here focus on the food part of changes in glucose levels, I am curious to know your thoughts on the stress part of glucose variability in patients.
Thanks for the kind words! Stress is definitely a major factor that leads to glucose variability and poor eating. Trying hard to diet or control one’s CGM can really add to that overall stress load. We encourage people to not try as hard – just follow the guidance of their premeal BG to validate their hunger and make better meal choices. Changing habits takes time. Unfortunately, most people burn out before they get the results they want and need.
Great review Marty. Your review made ALOT of sense. I’m happy that you took the time to write it. I just got her new book yesterday and going to read it in a little while. If I see that I’m not happy with it, I’ll return it. If you don’t mind, I have a question hoping you might be able to answer for me. I went LoCarb for about 1 year to get my blood sugars lower than what they are. (I’m not Diabetic but it runs in my family) I noticed that my readings are high in the morning even though I’m eating l Lo Carb. Is that normal? Also why would my blood sugar spike so much higher say if I ate a slice of pizza than someone who’s not eating LoCarb? Is it because my body chemistry isn’t the same anymore? If so how long would it take for my body to get used eating normal carbs without having those crazy spikes? Thanks and thanks again for this great review.
Great questions. Waking glucose is largely a function of body fat levels. People on a lower-carb diet tend to have higher waking glucose levels, but lower glucose during the day. Lowering waking glucose is really just a matter of losing some more body fat. See DDF FAQ 7.3 for some more details.
https://optimisingnutrition.com/understanding-your-unique-metabolism-ddf-faq-part-7/#htoc-7-3-what-is-a-healthy-waking-glucose-level
You may see a higher glucose level after eating carbs if you typically follow a low carb diet. If your pancreas is not used to pumping out as much glucose it can be sort of ‘surprised’ by a sudden massive bolus of carbs. If you needed to pass an oral glucose tolerance test for some reason, you could revert to a higher carb diet for a few days and you would go back to how you were before. Most people will see a LONG slowish rise in glucose that will last for many hours from pizza or other hyperpalatable fat+carb combos.