The monthly dance of hormones, cravings, and appetite in a woman’s body is nothing short of intriguing, and it captivates not just the curiosity of men but also that of most women.
The days leading up to menstruation bring with them a whirlwind of changes – increased cravings, appetite, fluctuations in blood glucose and insulin levels.
It’s a time when water weight gain and unpredictable emotions can seem like the norm. But here’s the silver lining: as menses arrive a few days later, all these changes reverse themselves.
This article delves deep into the intricacies of a woman’s body during her monthly cycle, deciphering what it’s striving to achieve. Instead of fighting against these natural processes, we aim to empower you with the knowledge to provide your body with precisely what it needs.
So, let’s dive into the remarkable world of the monthly hormonal cycle and discover how to harmonize your diet with the symphony of your body’s needs.
- The Monthly Hormonal Cycle
- Changes in Blood Glucose and Insulin
- What Can We Learn About Insulin and the Menstrual Cycle from People with Type 1 Diabetes?
- Diet Quality and Insulin Resistance
- Changes in Appetite and Cravings
- Why Do You Crave Chocolate at “That Time of the Month”?
- How Does My Metabolism Change Throughout the Month?
- Changes in Cravings for Nutrients
- Why do Some Women Lose their Period (Amenorrhea)?
- What Does This Mean for Fasting and Weight Loss?
- When Can I Push My Diet and Fasting Harder?
- What Should I Eat in Each Phase of My Cycle?
- Summary
The Monthly Hormonal Cycle
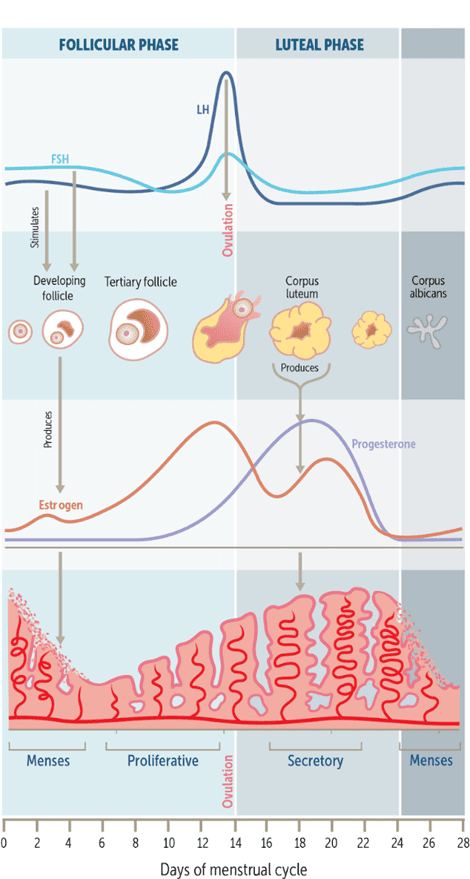
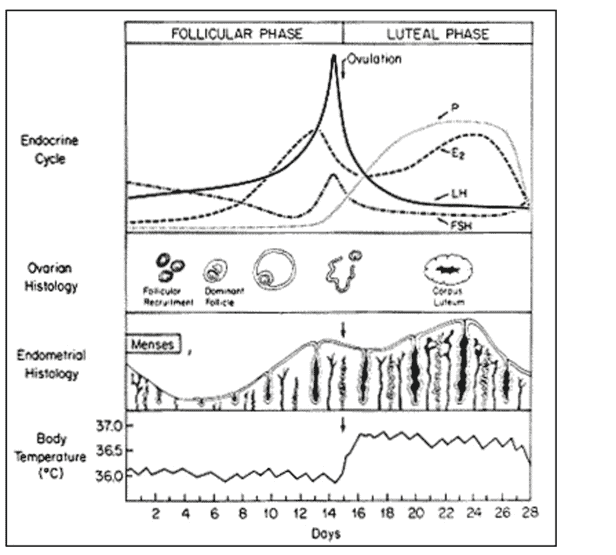
To set the scene, let’s first look at what is happening with your hormones.
- A typical cycle is approximately 28 days (although cycles lasting from 21 to 35 days are considered ‘normal’).
- ‘Day 0’ is the start of menses.
- Estrogen dominates the first half of the cycle, known as the follicular phase.
- Estrogen reaches its peak just before the halfway point of your cycle during ovulation.
- In addition to estrogen and progesterone, there is also a spike in testosterone around ovulation, making you feel a little friskier and sexier.
- During ovulation, an egg is released from the ovaries.
- The release of the egg at ovulation marks a transition from the follicular phase into the second part of your cycle, known as the luteal phase.
- Progesterone rules the luteal phase. Estrogen and progesterone rise again during this phase, and then both plummet before menses.
This cycle then repeats itself, continually building and breaking down to ensure your body is ready to support a new life.
You could liken your cycle to a monthly nutrition ‘cutting and bulking’ cycle: during menses, the uterus sheds its old lining (cutting). Things return to equilibrium for a few days.
Then, after ovulation, the body goes into growth mode to support a potential pregnancy after ovulation, just in case you’re pregnant (bulking).
Your cravings are your body’s way of ensuring it has enough energy and nutrients to nurture a growing foetus. It makes sense that your body requires a little extra fuel as it prepares to support a new life!
Changes in Blood Glucose and Insulin
Monthly changes in insulin give us a fascinating insight into what is happening across the monthly cycle.
Insulin is necessary to enable your body to grow (anabolic), but it is also critical to prevent your body from breaking down (anti-catabolic). If you had no insulin, your body would disintegrate.
Insulin is the signal from your pancreas to tell your liver to keep your stored energy from flowing into your bloodstream. The bigger you are, the more insulin you require to hold back more stored energy.
What Can We Learn About Insulin and the Menstrual Cycle from People with Type 1 Diabetes?
Menstruating women with Type-1 Diabetes give us a fascinating insight into how blood glucose and insulin levels vary through the monthly cycle.
The chart below shows my wife Monica’s total daily insulin doses averaged across twenty-nine monthly cycles. The fluctuations in insulin are due to both:
- insulin resistance from hormonal changes, particularly increased progesterone between ovulation and a couple of days before menses, and
- changes in appetite and food intake (more food requires more insulin, even if you eat minimal carbs).

The chart below shows Monica’s insulin during three phases of the cycle:
- menstruation (days 0 – 4),
- follicular phase, before ovulation (days 5 – 15), and
- luteal phase (days 16 – 25).
During menses, insulin drops to allow the uterine lining to break down (a catabolic process). Afterwards, insulin returns to normal levels until ovulation. Then, the body goes into anabolic overdrive growth mode between ovulation and a couple of days before menses (as if it were pregnant).
This increase in insulin resistance facilitates growth. If pregnancy occurs, insulin resistance increases for the next nine months.
To manage this in practice, I bump her basal insulin rates by 6% above the monthly average between days 16 and 25 and down by 4% for the rest of the month.
We also see a similar increase in insulin demand in rapidly growing teenagers who require insulin to facilitate growth.
In line with the elevated insulin levels, Monica often sees elevated blood glucose after ovulation in the latter half of the month, rapidly dropping just before the onset of menstruation.
In the Data-Driven Fasting app, you can flag your blood glucose if you notice it’s elevated leading up to menses. To account for this, the DDF app will raise your premeal blood glucose trigger to allow you to eat more regularly.
Swings in caloric intake around the monthly hormonal cycle tend to be more severe in women with polycystic ovarian syndrome (PCOS), which is linked to insulin resistance, T2D, and metabolic syndrome.
Before we dialled Monica’s insulin and blood sugars with better dietary choices and improved insulin management, her blood sugar and insulin swings were much larger.
Previously, she required up to 70 units of insulin per day and had an HBA1c of up to 11%. Her daily insulin demand is now in the low 30s, and her HBA1c is in the low 5s. As a result, her mood, sense of well-being, energy levels, and anxiety have all radically improved!
Diet Quality and Insulin Resistance
The study, Comparison of dietary micronutrient intake in PCOS patients with and without metabolic syndrome, found that women with PCOS tended to have lower intakes of antioxidant micronutrients like selenium, zinc, chromium, vitamin A, and vitamin E. The researchers concluded that a lower intake of these nutrients could contribute to insulin resistance and PCOS.
Diet quality and nutrient density are critical to minimising the negative impacts of the monthly hormonal cycle. In a food environment filled with ultra-processed foods, it’s understandable that monthly cravings can derail your best-laid plans.
However, if you can give your body what it needs when needed, you don’t need to be at the mercy of monthly hormonal swings. You can proactively ensure you get the nutrients from nutritious foods without resorting to less optimal choices.
Rather than mindlessly reaching for chocolate or junk food and chalking it up to being ‘that time of the month’, what if we could understand what the body is craving in terms of macronutrients and micronutrients and use them to design a dietary prescription for each phase of the monthly cycle?
Changes in Appetite and Cravings
Some recent research has given us some fascinating insights to help us understand what a woman’s body wants and needs throughout various phases of her cycle.
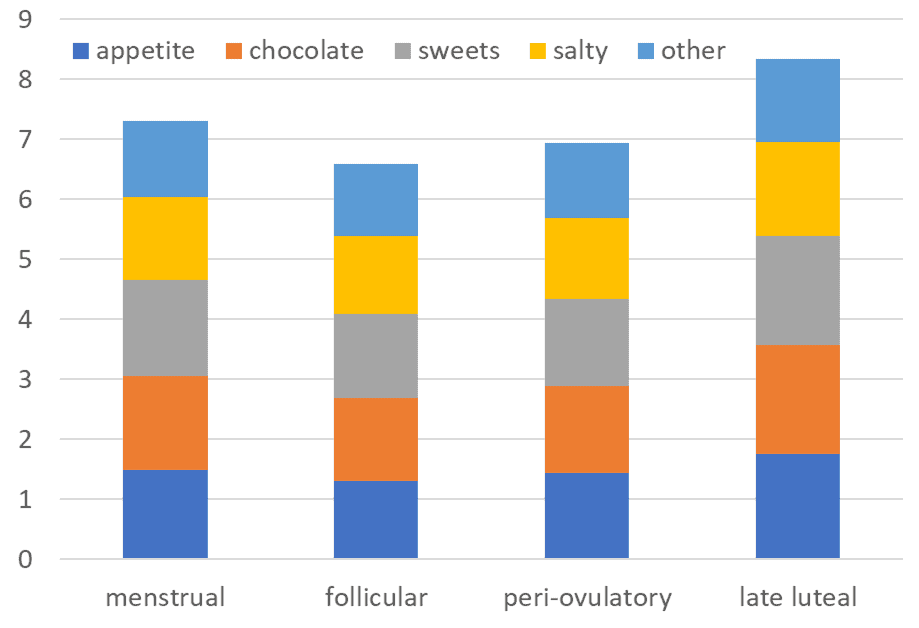
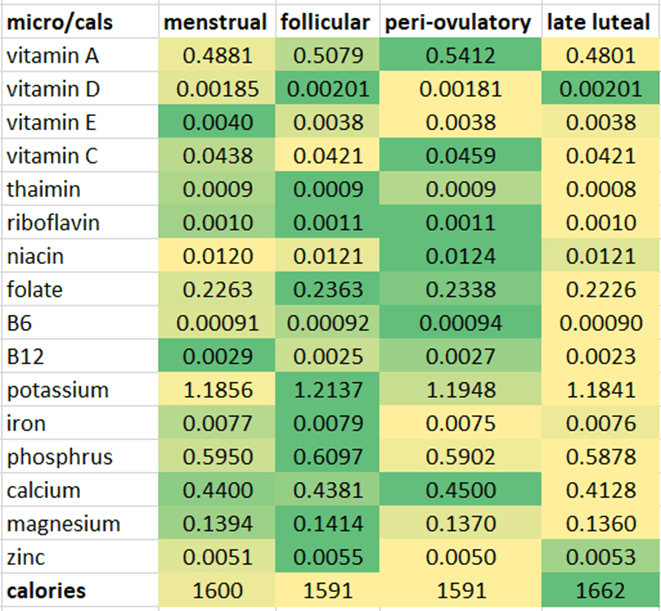
In the 2016 study, Changes in macronutrient, micronutrient, and food group intakes throughout the menstrual cycle in healthy, premenopausal women, researchers tracked the cravings and macronutrient and micronutrient intakes of 259 women across two cycles. They divided the monthly cycle into four phases and surveyed the women during each phase.
The chart below shows appetite and cravings peaked the week before menses and fell to their lowest before ovulation.
The study also found that total energy intake increased leading up to menses, with a statistically significant increase in total protein intake and protein %.
Protein intake from animal sources was also markedly higher during this time. There was also a substantial increase in cravings for foods containing the mineral zinc, which is critical for hormonal regulation and growth.
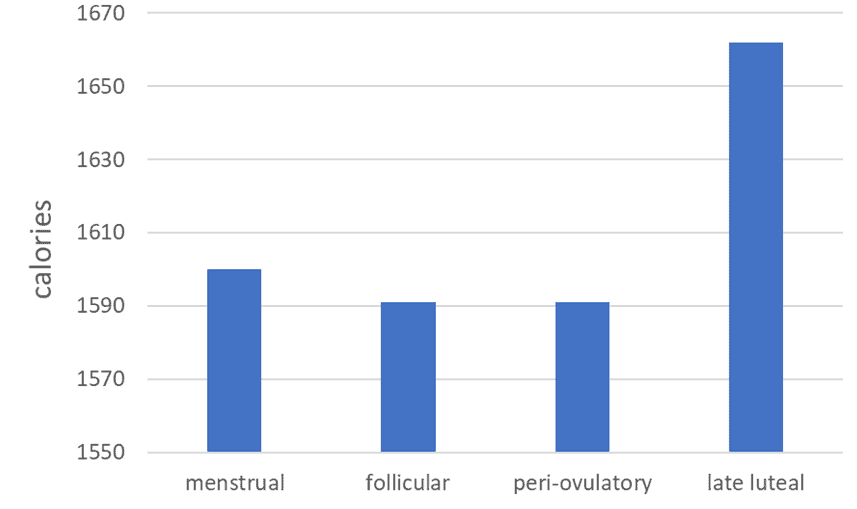
The chart below shows how calorie intake increases (by about 70 calories) just before menses. While insulin levels are at their lowest during menstruation to allow the uterine lining to break down, adequate energy and nutrients are still needed to replenish the losses.
It’s interesting to see that the change in calorie intake is similar to the increase in insulin (i.e. about 5%).
When we look at where the calories came from, we see that protein and fat increase a little before menses, with a slight decrease in carbohydrates.
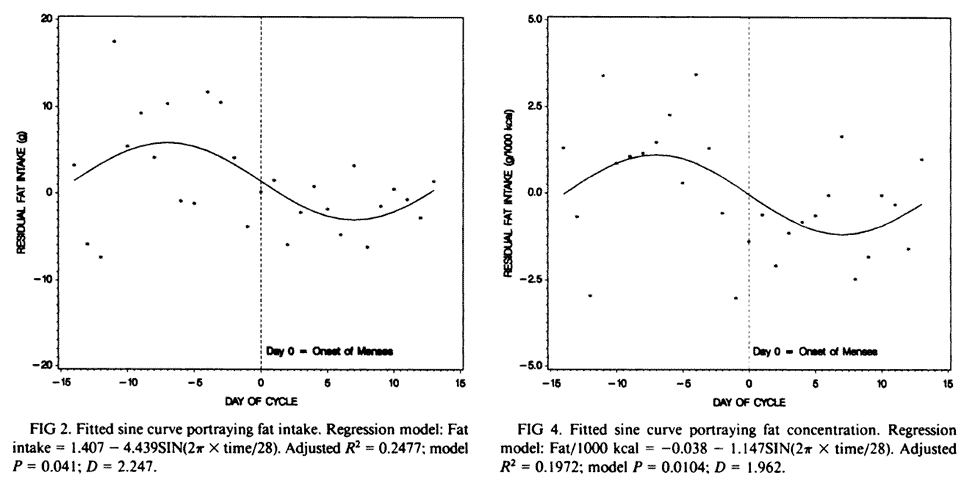
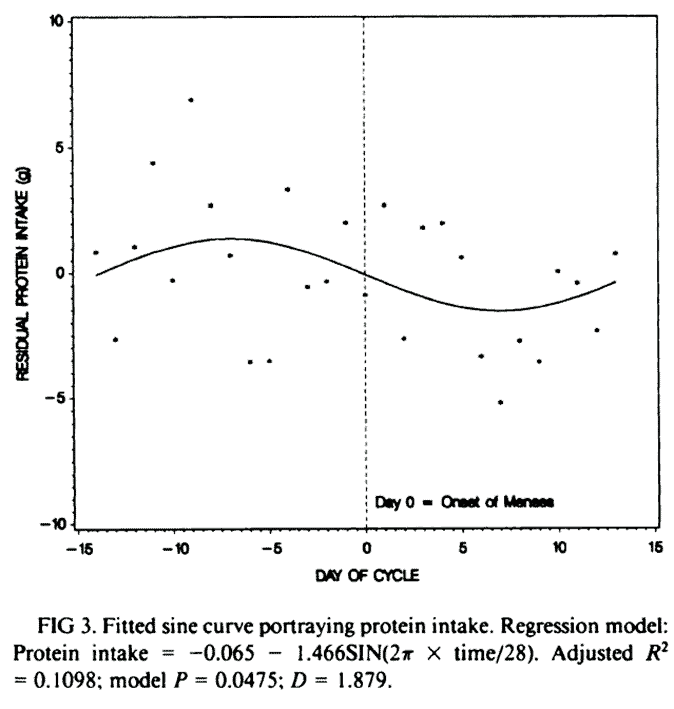
A separate study, Menstrual-cycle patterns in energy and macronutrient intake, also showed an increase in total energy in the days leading up to menses and a decrease afterwards.
Protein intake was also highest in the days leading up to menses. Protein plays a vital role in satiety, so if you don’t prioritise protein, you are more likely to binge on less-than-optimal fat+carb combo foods.
Fat intake (both in grams and per cent of caloric intake) was seen to peak before menses and decrease after that as the body seeks out energy-dense foods to support growth.
Why Do You Crave Chocolate at “That Time of the Month”?
Have you ever wondered why you crave chocolate in and around your cycle?
The cocoa in chocolate is rich in minerals like magnesium and copper, which regulate hormones. Chocolate is also energy-dense, meaning it gives you a quick energy hit and satisfies your need for more calories. Studies have also shown that chocolate can boost dopamine and serotonin levels, which fall in some women leading up to menstruation.
While there’s no harm in a bit of chocolate to crush those cravings, it’s ideal if you can proactively give your body more of what it needs.
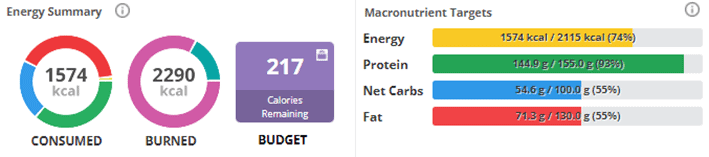
If you were tracking your calories (e.g., in our Macros Masterclass) to avoid binging on less optimal foods, you could bump up your energy limit by 50 – 100 calories per day while prioritising protein and nutrient-rich foods.
How Does My Metabolism Change Throughout the Month?
Because the hormones of a menstruating woman are constantly fluctuating, a woman’s metabolic rate is also changing. Progesterone, estrogen and even testosterone dictate how the reproductive system functions and burns calories. As a result, cravings for macronutrients, micronutrients, and food overall constantly change.
As the graph above from the study The Normal Menstrual Cycle and the Control of Ovulation illustrates, a woman’s metabolism is at its lowest during the first half of the cycle. As a result, she may not feel as hungry.
Body temperature increases considerably to sustain the implantation of an egg at ovulation. This rise in metabolic rate and temperature is another reason you may feel a little hungrier in and around ovulation.
Body temperature stays elevated during the luteal phase, as do progesterone, estrogen, and testosterone levels. This combination allows the metabolic rate to remain higher, which can also drive appetite.
Changes in Cravings for Nutrients
In the 2016 study, Changes in macronutrient, micronutrient, and food group intakes throughout the menstrual cycle in healthy, premenopausal women (discussed above), researchers also tried to identify micronutrient cravings.
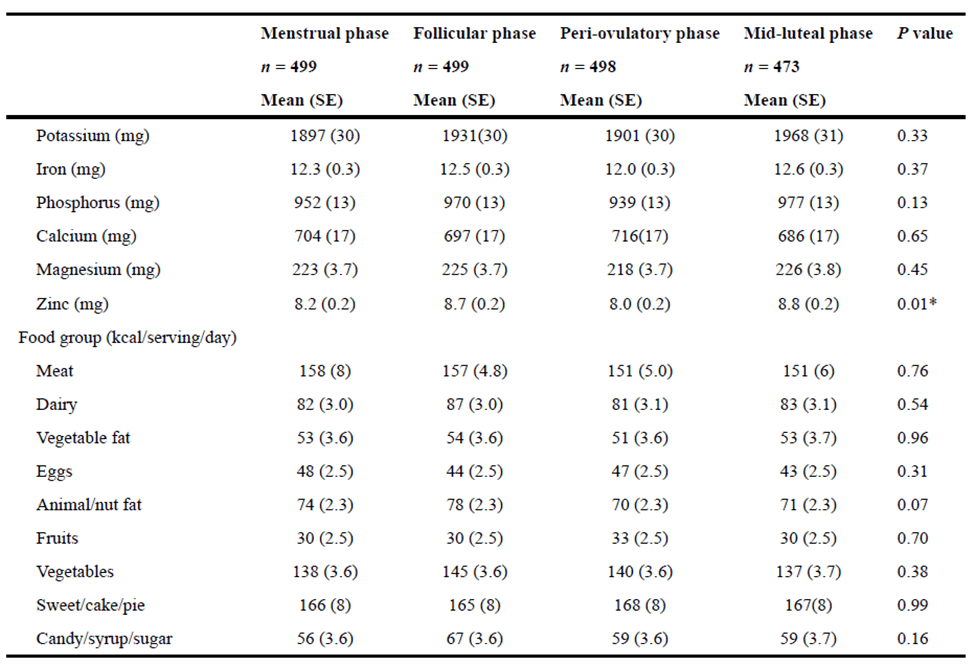
To dig a little deeper, I have divided the average intake of each nutrient in the study by the number of calories consumed during various phases of the menstrual cycle in the table below. In the table below, they are shaded from max (green) to minimum (yellow) for each micronutrient.
We can see that a woman’s body focuses on getting plenty of energy in the week before menses, with nutrient density being less of a priority (i.e., more yellow). However, more focus is on nutrients per calorie (nutrient density) in the first part of the cycle before ovulation (more green).
As outlined below, other studies have shown that various micronutrients are critical for a healthy hormonal cycle and help to reduce menstrual cycle symptoms.
Iron
Because there is considerable blood loss during menses, the body’s demand for iron increases to replace what has been lost, as a result, it seeks out food sources rich in iron (e.g., red meat).
Calcium
Calcium is a mineral we most often associate with bone health, but it can also help reduce premenstrual syndrome (PMS). In a study on the effects of calcium on premenstrual syndrome, there was a considerable decrease in period-related symptoms like anxiety, water retention, depression, and emotional changes.
Magnesium
Magnesium is necessary to process the overflow of hormones that occurs in and around menses.
Magnesium has been evaluated in a few studies that have proven effective at significantly reducing cycle-related symptoms.
Calcium is also is helpful for common and possibly debilitating cramps that occur during ‘that time of the month.’
In addition, zinc levels have been shown to fall during the second half of the luteal phase, and lower levels have been associated with PMS and PMDD. Other nutrients like iodine, omega-3 fatty acids, and various B vitamins (specifically B6) have also been shown to be effective at minimising signs and symptoms of premenstrual symptoms like water retention, mood changes, insomnia, and cramps.
Why do Some Women Lose their Period (Amenorrhea)?
A woman can lose her cycle by consuming an imbalanced amount of calories–either too few or too many. The chart below shows fertility, health and perceived attractiveness all align at a similar BMI – between the extremes of underweight and overweight.
Undernutrition
At one extreme, if a woman is not eating enough, her body loses its ability to reproduce from perceived starvation as it foregoes reproduction if enough calories aren’t available to support a new life. So, if you’re dieting and have lost your period, it’s a sign to take a break and eat more!
Overnutrition
At the other extreme, excess calorie consumption can also lead to a cycle loss. Overnutrition can cause insulin resistance and high insulin levels, throwing other hormones involved in reproduction out of balance.
Too Much Dietary Fat
Your body uses dietary fat to make sex hormones like estrogen, progesterone, and testosterone. If your fat intake is too low, the body has a hard time making them, and your cycle may become irregular.
While adequate dietary fat is essential, there’s no need to swing to the other extreme with excessive dietary fat. I’ve heard from some women who have lost their period on a very high-fat, low-protein ketogenic diet. Just like inadequate energy, your body knows it’s not a good time to procreate when there’s inadequate protein available to build a new life.
My friend Allison Herschede, who has Type 1 Diabetes and is a Diabetes Educator specialising in pregnancy for people with Type 1 Diabetes, said she experienced “severe mood swings, acne, extreme water retention and amenorrhea” when chasing ketones when keto was the exciting new craze in 2013. Her HbA1c went up to 8%, and her daily insulin requirements doubled during her 90% fat keto experimentation phase! Thankfully, her HbA1c has now returned to 4.8% with adequate protein and nutrients and a balanced eating routine with two solid meals a day.
Excess Cortisol
During times of stress, the body produces the stress hormone cortisol. This is fine over the short term, but high cortisol can have negative impacts when chronically elevated.
This is because cortisol ‘competes’ for synthesis with sex hormones. Cortisol keeps you alive, and reproduction becomes ‘optional’, so the body will prioritise making cortisol over sex hormones that support fertility.
Excess cortisol also tends to cause more testosterone to be converted into estrogen, a problem for both men and women.
Polycystic Ovarian Syndrome (PCOS)
Polycystic ovarian syndrome, or PCOS, is characterised by high androgens, anovulatory cycles, loss of fertility, ovarian cysts that rupture, and increased hair growth in women.
PCOS has strong links to obesity, general metabolic syndrome, Type-2 Diabetes, and insulin resistance. When the hormone insulin is constantly high from these conditions, the body can eliminate other hormones like those involved in reproduction. This can contribute to elevated androgens and resultant PCOS.
If you’re struggling with insulin resistance and elevated blood sugars, our Data-Driven Fasting Challenge is a great way to dial in your meal timing, lower your blood sugars, and lose weight in a wonderfully supportive community environment!
Endometriosis
Endometriosis is characterised by high estrogen levels, excessive and painful bleeds, pelvic pain from the build-up of scar tissue, infertility, pain with sex, and changes in sex drive.
Like PCOS, endometriosis is closely linked with metabolic syndrome, elevated blood sugars and insulin, and weight gain.
Hormones and fertility
If you’re looking to optimise or regain your fertility, hormone regulation is critical. Because the imbalance of hormones is often created by modern diet and lifestyle, a nutritious diet can help resolve amenorrhea, PCOS, and endometriosis.
What Does This Mean for Fasting and Weight Loss?
While many try to regulate their hormones with extended fasting, this might not be the best idea, particularly as they approach menopause.
Without first improving your nutrition, you may end up with excessive cravings that can lead to rebound binging on less-than-optimal foods, leading to worsening body composition and hormonal balance.
If you have lost your cycle (amenorrhea), or if it comes and goes, extended fasting is probably not ideal for you. Your cortisol may already be high, and the stress of missing a meal might push your “lizard brain” (amygdala) past its limits.
When Can I Push My Diet and Fasting Harder?
If you do have your cycle, you might be able to push a little harder with your fasting in the first half of the cycle when insulin levels and cravings are lower. Then, in the second half of your cycle after ovulation, you can dial it back a little and be gentler on your body, understanding that it is trying to gather nutrients to support a possible pregnancy.
In Data-Driven Fasting, this means you can push things a little harder before ovulation and wait until your blood sugar is below your personalised blood glucose trigger most of the time. Your blood sugars will tend to behave–at least until ovulation!
But after ovulation, you should give yourself a little more grace and focus more on giving your body the protein and nutrients it requires. Although you may see a bump in your weight (due to water retention) and blood sugars (due to temporary insulin resistance), you’ll be OK if you focus on the long-term trends.
What Should I Eat in Each Phase of My Cycle?
Although cravings can tell you if your body needs something, don’t mistake them for junk food cravings!
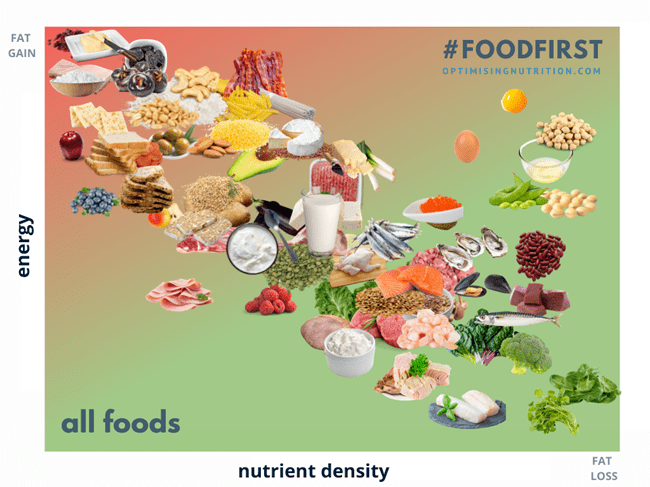
Hyperpalatable, chemical-rich foods have been engineered to baffle your taste buds into wanting more. However, shifting to a nutrient-dense diet focused on whole foods will ‘unclog’ your hunger cues and give you more reliable cravings.
To optimise your health throughout the month, it can be wise to match your meal choices to cycle with your hormones strategically. From ovulation to a couple of days before menses (i.e. days 16 – 25 of your cycle), you can allow your body a bit more energy (say 5%), knowing that it is trying to build for a possible pregnancy. However, in the rest of the cycle, you can focus more on food quality and work to use more stored energy if you are trying to lose weight.
Follicular Phase (Before Ovulation)
Your resting metabolic rate is at its lowest during the follicular phase, so you may find yourself less hungry! Higher estrogen levels will also help suppress your appetite. So, if you don’t feel particularly hungry, enjoy the ride while it lasts.
Blood sugar and insulin resistance are lower during the follicular phase, so, you might find you can tolerate carbohydrates without erratic spikes in blood sugar.
Because of the blood loss that comes with menstruation, it may be helpful to incorporate foods rich in bioavailable iron to replenish what has been lost. In addition, rebuilding the uterine lining that has just been shed also requires protein and fat.
In the days after your period, your body is not only recovering from a bleed but also trying to rebalance its hormone levels. So, make sure you’re well-hydrated with plenty of water and electrolytes like sodium, potassium, calcium, and magnesium to ensure hormones are not recirculated where they can contribute to hormone imbalance.
Consuming energy, particularly protein, should be a focus after ovulation. If your goal is weight loss, you can focus on nutrients (with less energy) before ovulation. In practice, this means you can go all out, focussing on nutrient-dense, high-satiety meals up until ovulation.
Luteal Phase (After Ovulation)
After ovulation, the body’s body temperature increases. The uterine lining also starts to thicken to support the implantation of a fertilised egg. This critical process requires energy and resources, so you will find yourself a little hungrier.
During the luteal phase, your body has a heightened demand for macronutrients like protein and fat to supply the raw ingredients it needs to prepare for a potential pregnancy.
Insulin and blood sugar levels increase, meaning carbs might not be as well-tolerated. Hence, responding to your cravings with excessive carb binges are more likely to put you on the blood sugar rollercoaster. This will leave you craving less optimal foods when your blood sugars come crashing down.
However, if you’re already following a low-carb diet or keto, this is not necessarily the time to restrict carbs even more, given your body needs a little more energy. Carbohydrates also help your body make more serotonin, which is critical to managing mood, PMS and your overall feeling of well-being at this time. If you’re active and need some carbs to stay fuelled, try consuming more fibre-rich or complex carbs to avoid blood sugar spikes.
In preparation for your upcoming period, it can also be helpful to prioritise foods rich in micronutrients like omega-3 fatty acids, vitamin B6, zinc, magnesium, and calcium that are helpful for symptoms like cramps, anxiety, bloating, water retention, and depression. In addition, iron-rich foods can also help prepare the body for its imminent blood loss, which leaves many women fatigued during and after menses.
Summary
A woman’s body goes through a monthly cycle of building up and breaking down.
Her appetite and cravings change to ensure she gets the nutrients she needs during each phase.
- In the time between ovulation and menses, she needs more energy to support the possible growth of a new life.
- From menses to ovulation, she can focus more on the nutrients she needs with less energy, particularly if she wants to lose weight.
Recipes Tailored to Your Monthly Cycle
The infographic below shows foods on the scale of nutrients vs energy. Before ovulation, you can push towards maximum nutrient density with less energy. However, after ovulation, you can retreat to foods a little more towards the upper left corner with more energy.
Over the last few years, we have created over 460 NutriBooster recipes across 27 recipe books to help you prioritise nutrient density with every meal.
The chart below shows how each of our NutriBosoter recipe books ranks in terms of nutrients vs energy.
- In the first half of your cycle leading up to ovulation, you can focus more on nutrient density (i.e., the NutriBooster books to the lower right corner of this chart).
- After ovulation, you can move more towards the upper left to account for increased energy demands.

The table below shows how you could use this approach for different contexts, with different NutriBoosters recipe books in the first and second phases of your cycle.
| Goal | Weight loss | Weight loss & blood sugar | Weight maintenance |
| Follicular phase (before ovulation) | High P:E Fat Loss Meat-based | Blood Sugar and Fat Loss | Maintenance |
| Luteal (after ovulation) | Maintenance | Blood sugar | Athletes & bulking Blood Sugar |
More
- Stress and Cortisol: The Missing Piece to Your Weight Loss and Blood Sugar Puzzle
- What Does Insulin Do in Your Body?
- What is Nutrient Density?
- Data-Driven Fasting: How to Lose Weight and Reverse Type 2 Diabetes Without Tracking Food
- Which NutriBooster Recipe Books is Right for Me?
- Macros Masterclass
- Intermittent Fasting Secrets for Women | Cynthia Thurlow
- Unlocking The Mysteries Of Female Hormones | Karen Martel








Great paper: very informative on every detail. So, for people like me who are healthy, well on weight, apply time restricted feeding and mostly eat low carb/keto in order to realize healthy ageing, but who may want to know more on whether their feeding could be even more optimized, what kind of course from your side would you consider to be optimal?
we have a number of courses for different people with different goals:
– Data-Driven Fasting is a great way to dial in when to eat (with a bit of what to eat) using a glucose meter as a fuel gauge – https://optimisingnutrition.com/data-driven-fasting/
– The Macros Masterclass guide people to dial in their macros, moving from where they are now towards optimal to align with their goal. The Macros Masterclass uses food tracking and optimal blood sugar tracking. – https://optimisingnutrition.com/macros-masterclass/
– Then we have the Micros Masterclass which guides people to dial in the nutrition at the micronutirent. Micros is a bit more intense, but takes nutrition to the ultimate level to ensure people get all the essential nutrients they need without excess energy. https://optimisingnutrition.com/all-about-the-micros-masterclass/
This is my favourite article by far, I understand my body better now.
Thank you Marty and the Team 🙂
thanks so much! I’m glad you found it useful!
This is my favourite article so far.
Thank you Marty and the Team 🙂